On this page
- What is this information about?
- Why have I been given this information?
- Will bottle feeding my baby mean I am still going to bond with them?
- Can I express my milk and give it in a bottle?
- What cues might my baby give me to show that they are hungry?
- How should I bottle feed my baby?
- What do I need to bring into hospital if I am bottle feeding?
- If I choose to give my baby formula milk, which should I choose?
- Is there an infant formula milk that is closest to breastmilk?
- What about infant formula milks that claim to help with hunger, colic, constipation, reflux, lactose intolerance or allergies?
- What do I need for bottle feeding at home?
- How long should I use infant formula for?
- How long should I express my milk for?
- How to make up a feed using powdered infant formula:
- How do I know if my baby is getting enough milk?
- Where can I look for more information and advice?
What is this information about?
This information is about bottle feeding your baby, with formula milk or expressed breast milk. It explains:
- how to spot when your baby is hungry, so you know when to offer them a bottle
- how to safely prepare a feed
- how to give your baby a bottle
- the difference between formula and breast milk
- how to know if your baby is getting enough milk.
Why have I been given this information?
If you are unable to fully breastfeed or decide to give your baby expressed breast milk or infant formula, this guide will support you to bottle feed as safely as possible.
It is important to be aware that formula milk does not provide the same benefits for you and your baby that breast milk can, such as protection against illness and infection.
You can keep this information in a safe place and share it with other people who are caring for your baby.
Will bottle feeding my baby mean I am still going to bond with them?
Yes. The early days with your baby are a great time to get to know and love each other. Keep them close, enjoy lots of skin-to-skin cuddles and follow the advice below when feeding.
All bottle-fed babies should be fed in a responsive way. This means following your baby’s cues (when they show you that they are hungry), rather than keeping to strict feeding times. Feeding responsively also allows your baby to drink as much and as quickly or slowly as they want. Over-feeding can make your baby feel uncomfortable and in pain. It could also lead to obesity (being very overweight) in childhood and later in life.
You will find more advice about the things your baby may do to show you that they are hungry in the information below.
Can I express my milk and give it in a bottle?
Yes. Breast milk can be collected by hand expressing (using your hands to gently squeeze milk out of your breast) or using a manual or electric pump. If you are breastfeeding, it is best to wait until your baby is feeding well before introducing a bottle.
It is best if babies are only breastfed or given breast milk for the first six months, and then have breast milk with solid foods until they are 2 years old and beyond.
Speak with your midwife or health visitor for more information or support with expressing.
What cues might my baby give me to show that they are hungry?
Feed your baby when they show signs of being hungry. This is called responsive bottle feeding. Cues can include:
- Moving their head
- Opening their mouth
- Sucking on their fingers
- Rooting (searching) for the breast
- Crying is the last sign of wanting to feed, so try and feed your baby before they cry.
How should I bottle feed my baby?
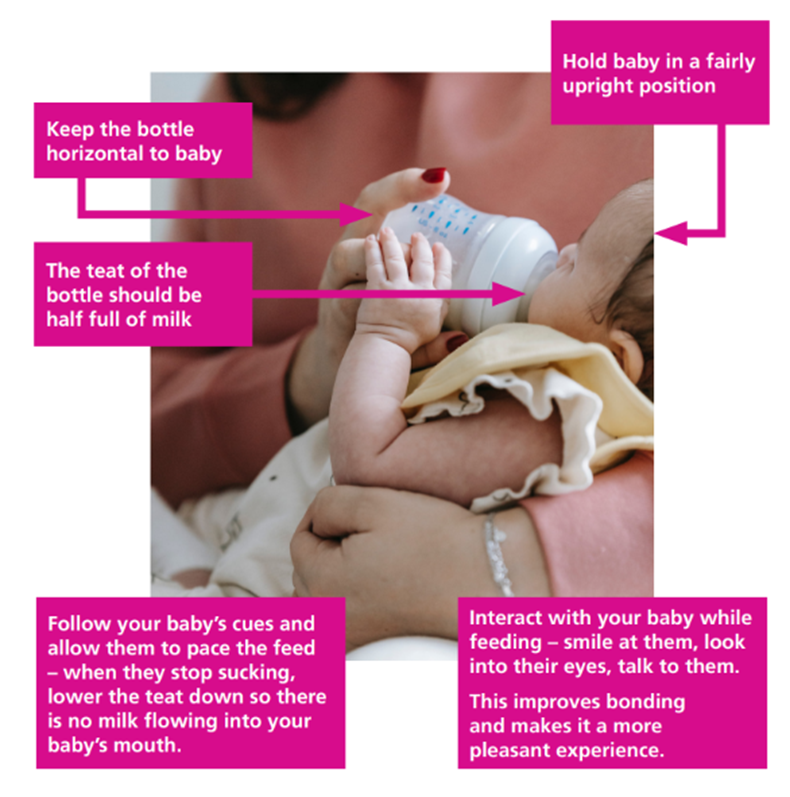
Babies will feel more secure if most feeds are given by the parents or primary (main) caregivers, especially in the early weeks and months. This will also help you to bond.
- Hold your baby close in an upright position so you can see their face and look into their eyes.
- Invite your baby to open their mouth by gently rubbing the bottle teat against their upper lip. When offering the teat, allow your baby to draw it further back into their mouth.
- Hold the bottle in a horizontal position (slightly tipped) to prevent milk from flowing too fast.
- Follow your baby’s cues and allow them to pace the feed and have a break when they need to. Signs will be different from one baby to the next. For example, they may:
- spread out their fingers and toes
- spill milk out of their mouth
- stop sucking
- turn their head
- push the bottle away
Gently remove the teat or bring the bottle downwards to cut off the flow of milk.
- Your baby will know how much milk they need at each feed. Forcing your baby to finish a feed can be a stressful experience and can mean your baby takes more than they need.
- Interact with your baby while feeding. Smile at them, look into their eyes, talk to them. This improves bonding and makes it a more pleasant experience.
- Alternate the side you hold your baby during feeds. This is good for your baby’s brain development.
What do I need to bring into hospital if I am bottle feeding?
If you choose to bottle feed with formula as soon as your baby is born, please bring in your own starter pack of ready-to-feed infant formula, suitable from birth. We do not supply infant formula in hospital unless it is needed for a medical reason. We can give you disposable sterile bottles and teats and we can sterilise equipment for you.
Small cartons or bottles of ready-to-feed formula are best, as milk can only be refrigerated for 24 hours once opened. You will need to bring ready-to-feed infant formula as we do not have the facilities to safely prepare or store powdered formula. Always choose first infant formula milk suitable from birth.
If you choose to bottle feed with expressed breast milk, we can give you colostrum syringes for hand expressing and we have hospital-grade pumps you can use while staying on the postnatal ward. You are welcome to bring in your own breast pump if you would like to.
If I choose to give my baby formula milk, which should I choose?
It does not matter which brand you use as they are all very similar, but it is important that it is a first milk infant formula. It does not matter if you choose cows’ or goats’ milk-based formula but talk to your midwife or health visitor before choosing soya-based.
You can continue to give this milk when your baby starts to have solid foods. It is not a good idea to give any other type of milk to young babies, such as ‘hungry baby formula’. Talk to your midwife or health visitor if you think your baby needs something other than first milk.
Find a simple, evidence-based guide to infant formula at First Steps Nutrition – visit: https://www.firststepsnutrition.org/parents-carers or scan the QR code below:
Is there an infant formula milk that is closest to breastmilk?
No. Breast milk cannot be copied. It is specially made by your body just for your baby, and it constantly changes to meet their needs. For example, breast milk changes depending on the time of day, your baby’s age, and even if either of you are exposed to illness. It contains special elements that help fight germs and boost immunity.
All infant formulas sold in the UK must meet strict nutritional standards, so they are all very similar and provide what your baby needs to grow and develop. Choosing a more expensive brand does not mean your baby will get extra health benefits. If any ingredient was proven to help babies, it would be added to all formulas by law.
What about infant formula milks that claim to help with hunger, colic, constipation, reflux, lactose intolerance or allergies?
Some of these infant formula milks are not evidence-based (based on good research) and might not be safe for your baby. If you think your baby may have a cow’s milk protein allergy, please speak with your GP. Special milks must be prescribed for your baby and should not be bought over the counter.
What do I need for bottle feeding at home?
You need to make sure you clean and sterilise all equipment to prevent your baby from getting infections and stomach upsets. You will need:
- bottles with teats and bottle covers
- bottle brush and teat brush
- sterilising equipment (such as a cold-water steriliser, microwave or steam steriliser)
- expressed breast milk, first infant formula powder or ready-to-feed liquid formula.
For information on how to sterilise and images of making up a feed, visit: NHS & Unicef ‘Guide to Bottle Feeding or scan the QR code below:
How long should I use infant formula for?
First milk formula should be used for the first year. There is no need to switch to follow-on milks.
When your baby is six months old, you can use small amounts of pasteurised whole cows’ milk when cooking and preparing foods.
Tap water is fine for infants over six months of age.
When your baby is one year old, they can drink full fat cow’s milk instead of formula milk.
How long should I express my milk for?
The longer your baby receives breast milk, the more protection and benefits for both you and your baby/babies. A single teaspoon of breast milk contains an estimated 3 million germ-killing cells and other immune-boosting factors. Breastfeeding or giving expressed milk for up to 2 years or longer is recommended for maximum benefits for both you and your baby.
How to make up a feed using powdered infant formula:
1. Fill the kettle
Fill the kettle with at least 1 litre of cold tap water. Do not use water that has been boiled before.
2. Boil the water
Boil the kettle. Let it cool for no more than 30 minutes. The water needs to stay hot (at least 70°C).
3. Clean your hands and surface
Wash your hands. Clean the area where you will make the bottle. This helps stop germs spreading.
4. Take the bottle out of the steriliser
If you use cold-water sterilising, shake off extra liquid. You can rinse the bottle with cooled boiled water from the kettle, not the tap.
5. Keep parts clean
Put the teat (the part your baby drinks from) and cap on the steriliser lid, not on the work surface.
6. Add hot water to the bottle
Follow the instructions on your baby formula. Pour the correct amount of boiled water into the bottle first. Check the water level is right.
7. Add the formula powder
Fill the scoop loosely, level it off with a clean, dry knife or the scoop leveller. Use the exact number of scoops in the instructions—no more, no less.
8. Put the bottle together and mix
Hold the edge of the ring and screw it on. Put the cap on and shake until the powder is mixed. If there are lots of bubbles, gently swirl the bottle.
9. Cool the bottle
Hold the bottom of the bottle under cold running water. Move it around to cool it evenly so it’s not too hot.
10. Check the temperature
Drop a little milk on the inside of your wrist. It should feel warm or cool—not hot.
11. Throw away leftovers
If there is milk left after feeding, do not save it. Throw it away.
12. Make bottles one at a time
To keep your baby safe, make each feed only when your baby needs it.
If you need to feed your baby formula away from home, follow the instructions on the NHS website below: Formula milk: common questions – NHS or scan the QR code:
How do I know if my baby is getting enough milk?
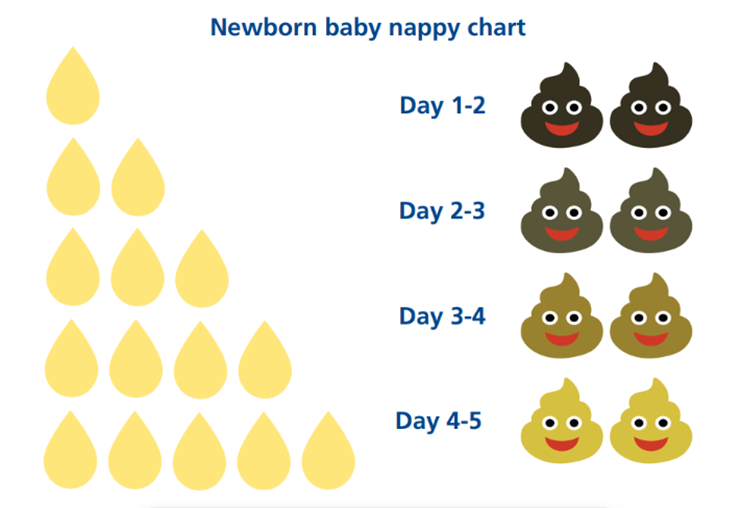
You can tell if your baby is getting enough milk by looking at their nappies. The guide below shows what you should expect to see.
1-2 days old:
- Wet nappies: 1-2 or more (you may see urates in their wee. This is a dark pink-red substance).
- Dirty nappies: At least 1, ‘tar-like’ poo, called meconium, in the first 24 hours, becoming less sticky and starting to change to brown/green by day 2.
3-4 days old:
- Wet nappies: 3 or more (nappies feel heavier).
- Dirty nappies: At least 2 poos that are changing from green to yellow. Please seek support from your midwife or infant feeding team if your baby’s poos are still dark in colour on day 3.
5-6 days old:
- Wet nappies: 5 or more (heavy wet).
- Dirty nappies: At least 2 yellow poos, may be quite watery.
7-28 days old:
- Wet nappies: 6 or more (heavy wet).
- Dirty nappies: At least 2, yellow and watery, and their poo looks a bit ‘seedy’.
Where can I look for more information and advice?
For further information and resources on infant feeding and nurturing your baby, please visit our ‘Flying Start’ padlet: https://padlet.com/uhsussexfeedingleads/flying-start-feeding-and-nurturing-your-baby-viqx4myf6rl48qkp or scan the QR code below:
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Today’s research is tomorrow’s treatments. That’s why UHSx is proud to be a research-active Trust. Find out how you can get involved.
Visit our website www.uhsussex.nhs.uk/research-and-innovation/information-for-patients-and-public or scan the QR code: