Download and print as a PDF (461kB pdf)
On this page
- What is sacrohysteropexy?
- Why do I need a sacrohysteropexy?
- What can I expect before the operation?
- What does the operation involve?
- What are the risks?
- What can I expect after the operation?
- What about going home?
- What about follow up?
- Are there any alternatives to having Sacrohysteropexy?
- Further sources of information
- Who can I contact with any concerns or questions?
What is sacrohysteropexy?
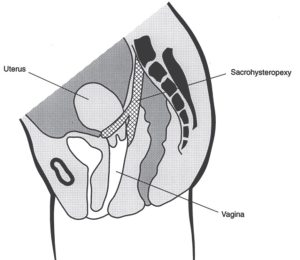
This is an operation carried out to correct uterine prolapse, in patients who do not wish to have hysterectomy. This is done by attaching the back of the cervix (neck of the womb) to the top of the lower back bone (sacrum).
Traditionally, mesh was used for this attachment. Although this use was never paused, during the mesh and tape pause that started in 2017, the concern about the use of mesh cannot be ignored. A strip of one of the layers of the abdominal (tummy) wall is used instead. As this is part of one’s own body, and not a foreign material, there are no concerns about its use.
It can be carried out under general or spinal anaesthesia. Associated prolapse of the vagina is dealt with at the same time.
Why do I need a sacrohysteropexy?
The operation is intended to support the uterus and correct associated vaginal prolapse. This is achieved by attaching the back of the cervix to the top of the lower back bone. This will improve associated urinary, bowel and / or sexual problems.
What can I expect before the operation?
At your pre op assessment and on your admission day the nurse will go through your hospital stay and explain your operation. Please do let us know about any concerns you have or if there is any information you think we should know about that will make your stay with us more comfortable.
You will need to make arrangements for your family, children or any other commitments that you have prior to coming in to hospital and to cover the length of your recovery.
You will see an anaesthetist and the doctor performing the surgery before you go to theatre. It is not unusual to feel anxious; the nursing staff will gladly discuss how you are feeling and talk you through your emotions.
If you have not already completed a quality of life questionnaire, you might be asked to do so before surgery. You will be provided with further copies to complete before your follow up appointment. This will help monitoring your progress before and after surgery. If you have not already signed the consent form on booking, the doctor will go through it with you before you go to theatre.
You will be asked for permission to enter your data on the national database for continence and prolapse surgery. This is a quality control measure to compare the safety and effectiveness of such procedures at the hospital against other units in the country.
What does the operation involve?
The operation is done through transverse incision through the abdominal wall and vaginal approach. The back of the cervix is lifted up and attached to the top of the lower back bone. This attachment is made using a strip of the tummy wall (rectus sheath).
A cut is made in the front and / or back walls of vagina to tighten the supporting layer around the bladder and / or bowel. The wounds are closed after that.
What are the risks?
There are risks with any operation but these are small. The main risks associated with a sacrocohysteropexy are:
Common risks:
- Postoperative pain
- Urinary tract infection. This may happen as a result of passing a catheter to drain the bladder. It is treated with antibiotics
- Wound infection, which may require antibiotics
- Bruising and delayed wound healing
- Initial difficulty in passing urine. This is usually managed by leaving a catheter to drain the bladder for longer and you can go home with a leg bag for few days. Less commonly, patients may need intermittent self catheterisation for a short period of time
Uncommon risks:
- The bladder and / or bowel rarely get injured during the operation and these are usually repaired at the time. If such injury is not identified and repaired at the time, there is a risk of fistula, but this is extremely rare
- Pelvic abscess or infection
- Late onset difficulty passing urine. This may manifest days or even weeks after being able to pass urine smoothly. The management is the same as initial difficulty passing urine, either by using a catheter with a leg bag and / or clean intermittent self catheterisation
- Deep vein thrombosis (blood clots in the leg veins) and pulmonary embolism (blood in the lung) can happen after any major operation. You will be asked to wear elastic stockings and given medication to prevent these clots
- The operation may fail or a prolapse may recur with time. This is rare as the operation is effective and durable to correct the condition
- Hernia at site of entry
- Haemorrhage requiring blood transfusion. Sometimes, bleeding only becomes apparent after surgery and requires returning back to theatre
- Whilst the operation may improve the sense of bulge, there is small chance that urinary, bowel and / or sexual problems may persist. It is hoped however they will at least improve to some degree
- Unmasking of stress incontinence of urine. Uterine prolapse may lead to urethral kink, hiding bladder neck weakness. Correcting the prolapse will straighten the urethra, revealing any weakness that was hidden. Stress incontinence is first managed by pelvic floor exercises. If it persists despite these exercises, an operation to improve continence is carried out
In order for you to make an informed choice about your surgery please ask one of the doctors or nurses if you have any questions about the operation before signing the consent form.
What can I expect after the operation?
As you come round from the anaesthetic, you may experience episodes of pain and / or nausea. Please let the nursing staff know and they will assess you and take appropriate action. A small drain may be placed in the abdominal wound to remove any excess blood.
A catheter to drain the bladder is inserted into the bladder to save you having to go to the toilet, till you are fully mobile after the operation. You may have a pack in the vagina. You will have a drip to give you fluids, though you will be able to eat and drink. You may have a PCA pump (Patient Controlled Analgesia) to control your pain. This is not common and will be discussed with you before the operation by the anaesthetist.
The nurses will assess you regularly to ensure that the PCA is effective. We will use a pain score to assess your pain (0 to 10; 0 = No Pain, 10 = Very Strong Pain).
Your nurse will be checking your blood pressure, pulse, breathing and temperature and monitor the wound across your abdomen and any vaginal bleeding. S/he will also ask you to move from side to side and to do leg and breathing exercises once you are able, this will help prevent any pressure damage, a DVT (deep vein thrombosis) or chest infection.
The first 12 hours after the operation
You can expect pain and discomfort in your lower abdomen for the first few days after the operation. You may also experience pain and will be given pain killers to alleviate this.
Day 1 after the operation
The drain, drip, vaginal pack and catheter that drains the bladder are usually removed the next day. The nursing staff will assist with washing as necessary and encourage early mobilisation. We would normally expect you to sit out of bed and begin to walk around the day after your operation.
You will be able to go home when you are passing urine without difficulty. You will be asked to pass urine in a jug and will have a scan to measure how much urine is left in the bladder. The key to the success in this respect is to forget that you need to pass urine and drink and walk as you would normally do, and this when your bladder is likely to work as normal.
You will have a dressing on the wound across your abdomen that will be removed the day after your operation and you will be able to shower. You may also find it difficult to open your bowels at first, we will give you mild laxatives to soften your stools and prevent constipation and straining.
What about going home?
You will be seen and assessed by the gynaecology team the following day to check on your recovery and decisions will be made about your care, this information will be shared with you. You may then be able to go home.
Please feel free to ask questions about your operation and recovery at any time.
The average length of stay following sacrohysteropexy is 1 to 3 days. Most patients go home on the second post-operative day. As you physically recover from your operation, the nursing team will discuss your convalescence. To ensure you have a good recovery you should take note of the following:
Rest
During the first two weeks at home it is common to feel tired, exhausted and emotional. You should relax during the day gradually increasing the number of things you do each day. Avoid crossing your legs when you are lying down.
Vaginal bleeding
You can expect to have some vaginal discharge / bleeding for few days after surgery. This is like a light period and is red or brown in colour. Sanitary towels should be used, rather than tampons, to reduce the risk of infection.
Stitches
The wound across your abdomen will be closed by dissolvable stitches. If after 7 days you notice the stitches have not dissolved then they will need to be removed. This is normally done by your practice nurse, but you will need to make an appointment. We advise that you shower daily and keep the wound clean and dry. There is no need to cover the wound with a dressing. The wound(s) inside the vagina are also closed with dissolvable sutures as well.
Housework:
Weeks 1 to 2
We recommend that you do light activities around the house and avoid any heavy lifting (not more than 1.5kgs in each hand).
Weeks 3 to 4
We recommend that you gradually introduce lighter household chores, dusting, washing up, making beds and ironing. You may begin to prepare food and cook remembering not to lift any heavy items.
Weeks 4 to 6
By this time you should resume normal daily activities, but continue to refrain from straining till 3 months after surgery, to ensure good healing.
Exercise
Exercise is important and it is advisable to go for short walks each day, increasing the distance gradually. You should avoid straining or heavy exercise for 3 months, to ensure good healing of the sling. You may return to light exercise, like gentle cycling and swimming after 4 to 6 weeks. You will be able to manage the stairs on your arrival home. We encourage you to do pelvic floor exercises. You will be given a physiotherapy booklet titled ‘Fit for Life’ to guide you.
Diet
A well balanced nutritious diet with high fibre content is essential to avoid constipation. Your bowels may take some time to return to normal after your operation and you may need to take laxatives. You should include at least 5 portions of fruit and vegetables per day. You should aim to drink at least 2 litres of water per day.
Sex
You should usually allow 4 to 6 weeks after the operation before having sex to allow the vaginal scar to heal. If you experience vaginal dryness, you may wish to try a vaginal lubricant from your local pharmacy. If after this time you are experiencing pain or any problems with intercourse then you should see your GP.
Returning to work
This will depend on the nature of your work. If you work in an office base environment, you will need 4 to 6 weeks off work. If your work involves lifting and exertion, you will need 3 months off work. The hospital doctor will provide a sick certificate for this period.
Driving
It is usually safe to drive after 12 weeks but this will depend on your level of concentration, ability to perform an emergency stop and your car insurance policy.
What about follow up?
You will be invited for follow up, usually about 12 weeks after surgery. If you have problems before this, you can contact your doctor or contact the hospital to bring the appointment forwards. During this follow up appointment, your symptoms will be reviewed and you will be examined to assess wound healing. The quality of life will be checked.
Are there any alternatives to having Sacrohysteropexy?
You may decide not to have surgery and want to try vaginal pessaries to control the prolapse without having to have an operation.
Alternative forms of surgery include:
- Laparoscopic sacrohysteropexy, which is the same operation performed through key hole
- Vaginal repair with sacroscpinous hysteropexy. In this operation, the prolapse is corrected vaginally and the back of the uterus is fixed to a ligament in the pelvis
These can be discussed with your doctor.
Further sources of information
British Society of Urogynaecology: Sacrohysteropexy for
Uterine Prolapse leaflet
NHS.uk: Pelvic organ prolapse treatment
NICE guidelines: Uterine suspension using mesh (including sacrohysteropexy) to repair uterine prolapse
Who can I contact with any concerns or questions?
You should contact your GP or the hospital if you notice increased temperature, wound swelling and / or pain, smelling discharge either from the wound or the front passage, blood in urine or motion, abdominal distension and / or failure to open your bowel.
If you have any problems or questions, please use the telephone numbers to contact us.
Princess Royal Hospital
01444 441881
Ext. 5686
Royal Sussex County Hospital
01273 696955
Ext. 4013
Urogynaecology Unit at Lewes Victoria Hospital
01273 474153
Ext. 2178
This patient information leaflet was prepared by Dr. Sharif Ismail, Consultant Subspecialist Urogynaecologist.
This information leaflet has been approved at the Clinical Governance and Safety and Quality Meetings of the Department of Obstetrics and Gynaecology as well as Brighton and Sussex University Hospitals NHS Trust Carer and Patient Information Group (CPIG).
Ratified April 2017 Women’s Safety and Quality Committee.
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.