Download and print as a PDF (465kB pdf)
On this page
- What is an ERCP?
- How do I prepare for my procedure?
- What should I bring with me to the unit?
- Can I park at the hospital?
- What happens when I arrive in reception?
- What are the benefits?
- Are there any significant risks?
- What happens after my examination / procedure?
- Frequently asked questions
- Your comments and suggestions
What is an ERCP?
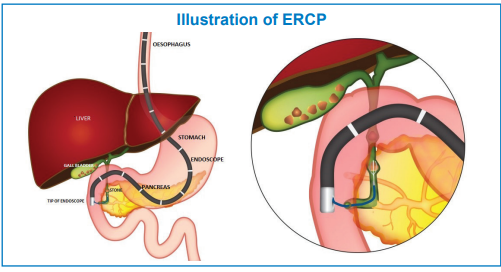
ERCP (endoscopic retrograde cholangio-pancreatography) is a procedure which enables the endoscopist to examine the bile duct and / or pancreas. This will involve the use of x-rays. The amount of x-rays you receive will be strictly controlled for your safety. The staff will be wearing x-ray protective aprons because of their repeated exposure to x-rays.
You will be given sedation and painkiller before an endoscope (a flexible camera tube) is carefully passed into your mouth, down your gullet through your stomach and into the beginning of the small intestine (duodenum).
By using the endoscope, the doctor can examine the opening of the bile duct. A small plastic tube can be passed down the endoscope into this opening (called the papilla) and dye injected into the bile ducts, enabling x-ray pictures to be taken.
If a gallstone (or some other blockage) is found, it can be treated first by making a small cut in the papilla and removing the stone, or by placing a stent to relieve the blockage. You will find a more detailed explanation of this a bit further on in this booklet.
How do I prepare for my procedure?
- Have nothing to eat, and do not drink milk, for 6 hours before your appointment.
- Have nothing to drink for 2 hours before your appointment.
- Please contact your GP surgery or nurse specialist if you are diabetic and need advice regarding your medication.
- Please contact the endoscopy unit if you take warfarin or any other anticoagulant or anti-platelet medicine
What should I bring with me to the unit?
- Because you will be having sedation for your procedure, you will need someone to act as an escort and stay with you for the remainder of the day and overnight. Your escort must come up to the unit to collect you. We cannot take you down to meet them
- A list of all your medication
- Your reading glasses
- Wear loose and comfortable clothing
- Do not bring any valuables with you
Can I park at the hospital?
Parking space at the Royal Sussex County Hospital is very limited, so please set off in plenty of time for your appointment and be prepared to wait in the car park queue. Alternatively, your escort may drop you off at the Millenium Wing and then return to the unit to collect you later.
It is very important that you follow all the instructions carefully, or your examination may need to be postponed.
What happens when I arrive in reception?
Please report to the desk. Our receptionist will check your details and ask you to take a seat in the waiting room. You will then be called through by a nurse or health care assistant, who will explain the examination / procedure to you and ask you some questions about your medical history. If you are having sedation, please ensure that you have your escort’s contact details with you so that we can call them when you are ready to be collected. If you have any questions or if there is anything at all that you don’t understand, please ask. You will be asked to sign a consent form before the examination / procedure. Please see a copy of the form at the back of this booklet.
What are the benefits?
If the x rays show a gallstone or a blockage, it will be treated immediately using one of the following methods:
Endoscopic sphincterotomy
This procedure will be carried out if a gallstone is found. The doctor will enlarge the opening of the bile duct (sphincterotomy), using an electrically heated wire (diathermy) which you should not feel. Any stones can then be collected into a tiny basket and left to pass into the intestine.
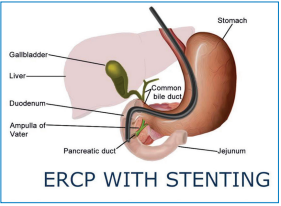
Endoprosthesis
If the x rays show a blockage in the bile duct, the doctor may place an endoprosthesis (a tiny plastic tube called a stent) inside the bile duct itself to help the bile to drain away into the intestine in the normal way. This may be removed at a later date.
Spyglass
This procedure will be performed if a gallstone is too large to remove by other methods, or if there is a narrowing or blockage which requires direct visualisation and a sample of tissue being taken. The spyglass is a small camera which is passed through the endoscope into the bile duct. It allows direct visualisation, lithotripsy (destruction of the stone/s using shockwaves) or biopsy to be performed. The stones/fragments are then removed from the bile duct and pass into the bowel naturally. The biopsy is sent to the laboratory to be analysed in the normal way.
Are there any significant risks?
This treatment for bile duct stones and blockages has been developed and is recommended to you because it is simpler and safer than surgery. However, you should be aware that it is not always successful and that occasionally problems can arise. In around 2% of patients who are treated for gallstones by endoscopic sphincterotomy, bleeding occurs from the incision of the bile duct. If bleeding does occur, it will usually stop within 24 hours. On rare occasions however, it may require an operation. Up to 5% of patients may develop pancreatitis – a painful inflammation or irritation of the pancreas. This will usually resolve itself within a few days. Very rarely, it can be life threatening, and may require an operation. Please speak to the doctor or nurse performing your procedure if you have any concerns.
There is a risk of infection following the use of spyglass cholangioscopy due to the instrumentation in the bile ducts. The infection is called cholangitis. To reduce this risk antibiotics will be given during the procedure.
What happens after my examination / procedure?
You will be taken into recovery and will be given time to rest. The nurses will check your vital signs regularly. You will not be able to have anything to eat or drink for up to 2 hours afterwards. If you have a gluten allergy please bring something to eat. You will need to rest for the remainder of the day and refrain from smoking, and drinking alcohol. You MUST NOT drive, sign legal documents or operate any machinery for 24 hours. Before you leave the unit an explanation of the findings will be given to you, and your GP will receive a copy of the report.
Frequently asked questions
Will it hurt?
Endoscopic examinations and procedures can be uncomfortable, so we have a variety of interventions at our disposal to make it more comfortable for you. Sedation and intravenous pain killers will be given for ERCP. Please let us know if you are uncomfortable in any way and we will do our best to help you. After an ERCP you may suffer from a sore throat and bloating. These effects should disappear after a few days but you will be given written aftercare advice when you go home, which tells you what to do if your symptoms do not settle.
How long will it take?
Examination / procedure times vary. A simple diagnostic examination should take between 10 and 30 minutes but a more complicated examination, involving endoscopic treatment, can take anything from 30 minutes to 90 minutes, or longer. Your recovery time will also be slightly longer. This is why you should be prepared to be in the unit for possibly 3 to 4 hours.
When will I get my results?
Biopsy results may take up to 8 weeks to come back from the laboratory. The findings are reviewed by your consultant, who will then arrange follow up. This could be a clinic appointment to discuss your results or it could be a letter explaining your results. Please do not phone our recovery area during this time – we are unable to give any biopsy results over the telephone. If you have not heard anything after 8 weeks, and you are worried, please contact your GP, who will be informed of your results.
What do I do if I need to cancel or change my appointment?
If you need to cancel or change your appointment please call us on 0300 303 8517.
Your comments and suggestions
If you have any concerns about your treatment or care, please bring them to our attention. We will do our best to help. If you feel you would like some support with raising your concerns, the Patient’s Advocate is available to speak on your behalf. You can contact the Patient’s Advocate by telephone between 10am and 4pm on:
Princess Royal Hospital
01444 441881
Ext. 65909
Royal Sussex County Hospital
01273 696955
Ext. 64029 or 64588
Email: [email protected] for either site.
We always welcome new ideas and suggestions. Please let us know if you feel there are ways in which we could improve our service.
At the end of the leaflet is an example of the form ‘Patient agreement to investigation or treatment’. Please print off the PDF version to obtain the example form.
Thank you for taking the time to read this information. If there is anything at all that you don’t understand, or you have any questions, please ask a nurse at the unit or call us.
Royal Sussex County Hospital
01273 696955
Ext. 64570
Princess Royal Hospital
01444 441881
Ext. 68187
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information here is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.