Download and print as a PDF (166kB pdf)
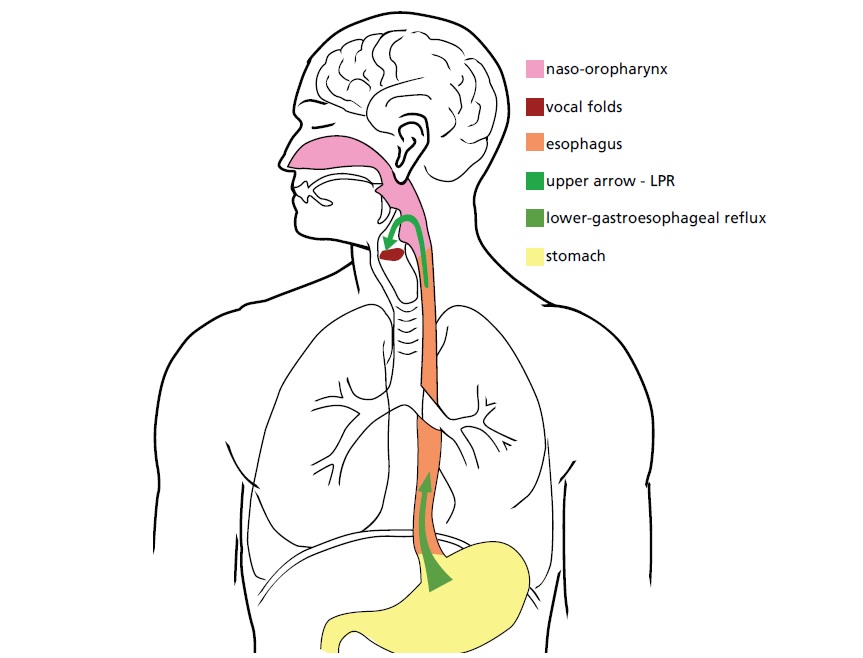
In some people the stomach acid or the stomach contents may come up into the throat and/or gullet connecting the throat to the stomach. This may occur at any time day or night, but is most common after meals and when lying down.
Symptoms include recurrent coughing, sore throat, heartburn or indigestion, excessive mucus or post nasal drip, an unpleasant taste, or a sensation of a lump in the throat.
This advice is designed to help neutralise the stomach acid, reduce the production of acid, and prevent acid from coming up into the oesophagus or gullet. You should adopt enough of these suggestions to get relief from your symptoms. Healing of the irritated oesophagus and throat will take time, and you should allow at least four to six weeks of careful treatment before expecting results and relief from symptoms.
On this page
What causes it?
Reflux may be caused, or increased, by what we eat and/or drink, how we eat and drink, our lifestyles and medicines we take.
What can I do to help?
There are many things you can do to help reduce the risk, frequency and/or severity of attacks of acid reflux.
Food and drink
- Eat smaller, more frequent meals, rather than starving yourself then eating a big meal
- Eat less in the evening and leave at least two hours between your last meal and going to bed
- Avoid eating ‘on the run’
- Sit upright when eating; don’t sit in a low armchair with a tray on your lap
- Try to remain upright at least one hour after eating. Avoid slumping or bending over after eating
- Drink plenty of water
Food to avoid
- Hot, spicy food, tomato based foods, onions, citrus fruits, juices, anything with vinegar
- Fried, fatty or greasy foods
- Caffeinated and decaffeinated coffee, tea
- Chocolate
- Carbonated (fizzy) drinks
- Alcohol
- Very salty, crispy or crumbly foods. These may increase the irritation already caused by the reflux
Lifestyle
- Avoid wearing tight clothing around your middle
- Avoid stressful situations if you can and do things to help you to relax such as joining relaxation classes, doing yoga or going swimming
- If you smoke, give up. For more information on giving up smoking, please call the NHS Smoking Helpline on 0800 0224332
- Raise the head end of your bed by putting blocks underneath, 10 to 25 cm high. Just using more pillows will not do the trick
- If you are overweight, ask your doctor for some help and advice about losing weight
- It is better to sleep on the left side or on the stomach, to allow gas to escape from the stomach and reduce the escape of acid material
Medicines
Certain medicines may increase your risk of getting acid reflux. These include:
- Some tranquilisers
- Steroids
- Some medicines taken for asthma
- Large dose vitamin C (1,000mg)
- Beta blockers
- Tablets containing progesterone
- Aspirin
Do not stop taking medicines you have been prescribed, but ask your GP or pharmacist for advice if you think your medication is contributing to reflux.
Antacids
Antacids such as Rennies are available without prescription at your local pharmacist. Antacids can interfere with the absorption of certain drugs, and it is therefore important to be aware of this side effect. In the beginning, you may wish to take an antacid just at bedtime, but if symptoms are very persistent, they can be taken 45 minutes after eating, every two hours between meals, and at bedtime.
Gaviscon is not antacid, but floats on top of the stomach acid, preventing oesophageal irritation, and is often found to be very helpful when taken regularly after meals and at bedtime. You can buy this from over the counter.
Where can I get further information?
NHS Choices provides online information and guidance on all aspects of health and healthcare, to help you make choices about your health.
Who can I contact with any concerns or questions?
If you have any problems or are worried, please do not hesitate to contact us at:
Royal Sussex County Hospital
ENT Outpatient Department
01273 696955
Ext. 64813
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.