This leaflet helps you understand bile salt diarrhoea and outlines the treatments and practical steps that can improve your symptoms.
Download and print as a PDF (652kB pdf)
On this page
What is this information about?
This leaflet gives you advice about bile salt diarrhoea (also called bile acid or bile salt malabsorption).
It explains:
- what it is
- why it happens
- the symptoms
- how it can be treated
Why have I been given this information?
You have been given this leaflet because your team thinks bile salt diarrhoea may be the cause of your symptoms. Following this advice can help you understand your condition and know what treatments are available.
What is bile salt diarrhoea?
Bile salt diarrhoea is sometimes called bile salt malabsorption or bile acid malabsorption. These terms all mean the same thing. In this leaflet, we use the term bile salt diarrhoea.
Bile salts are chemicals made in your liver that help you digest food, especially fat. When you eat, bile salts are released from your liver and gallbladder into your small intestine. Normally, they are absorbed back into your body in the last part of the small intestine (the terminal ileum).
If this reabsorption does not happen, the bile salts move into your large bowel (colon), where they pull in water and cause ongoing diarrhoea.
Why do I have bile salt diarrhoea?
There are three main reasons:
- Type 1: Problems with the small intestine or ileum – for example, after surgery for Crohn’s disease or cancer, or when the bowel is inflamed.
- Type 2: No clear cause – this is called idiopathic or primary bile salt diarrhoea, and it is the most common type.
- Type 3: Other gut conditions – such as coeliac disease, pancreatitis, gallbladder removal, radiotherapy, or peptic ulcer surgery.
What are the symptoms?
People with bile salt diarrhoea may:
- Need to rush to the toilet, often soon after eating
- Pass watery, pale stools (poo)
- Have tummy cramps and smelly wind
- May go to the toilet more than 10 times a day
- Feel anxious about leaving home due to diarrhoea
- May lose weight over time
Because vitamin B12 is also absorbed in the ileum, you may also develop a vitamin B12 deficiency. This could cause effects such as feeling weak or tired, headaches, upset stomach, problems with vision, sore tongue/mouth, problems with memory, understanding and judgement, numbness and problems with balance and coordination. A simple blood test can check your levels to see if you need supplements.
How is it treated?
1. Treating underlying causes
If another condition (such as Crohn’s or coeliac disease) is causing your symptoms, treating that condition can improve your diarrhoea.
2. Low-fat diet
All types of bile salt diarrhoea can be eased by a low-fat diet. In mild cases, this may be enough on its own.
Tips for a low-fat diet:
- aim for less than 40g of fat a day
- limit butter, spreads, and oils to 3 teaspoons (15 mls) daily
- avoid frying. Instead, grill, boil, steam, microwave or dry roast food
- choose lean meat and low-fat dairy products
- ask your team for a referral to a dietitian if needed
3. Medicines (bile acid sequestrants)
If diet changes do not help, medicines can bind bile salts in your gut, stopping them from drawing water into your bowel.
These medications are called bile acid sequestrants.
Be aware,
there are 2 types of bile acid sequestrants available.
Both are ‘off-label’ for bile acid diarrhoea use. ‘
Off-label’ means that the medicine is being used in a way that is different to that in the license. We have a lot of positive experience in using them. If you have any questions about this, please discuss with your specialist team.
The two medicines most used are:
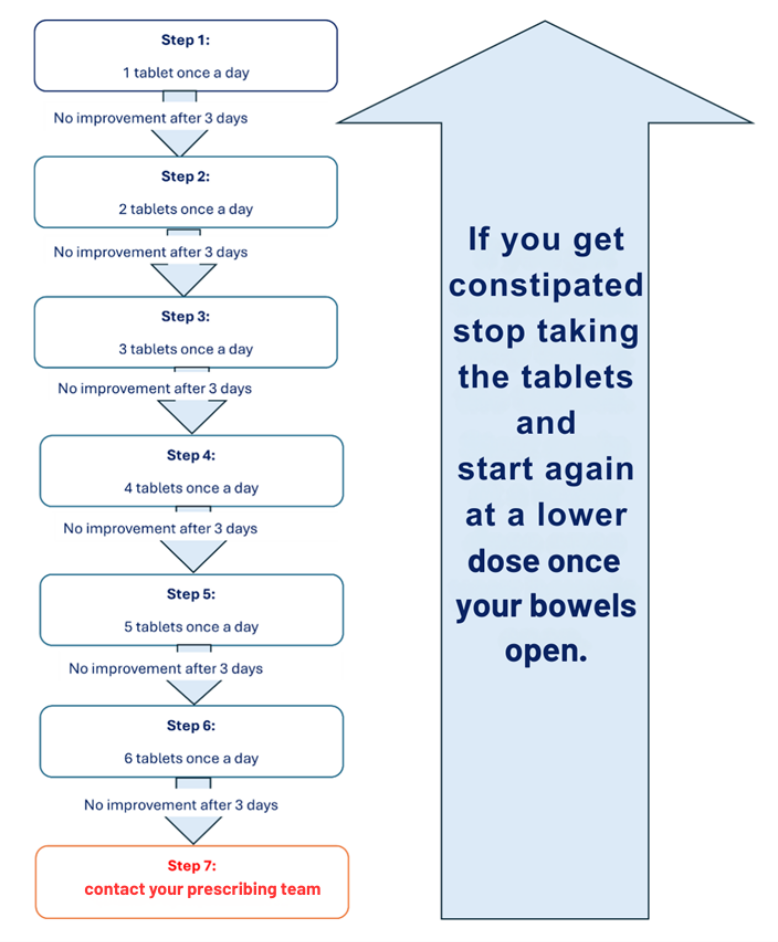
- Colesevelam (tablets)
- Start with a low dose and increase slowly to avoid constipation (see flow chart)
- Take once a day, at least 4 hours before and after other medicines
- Works well if taken at lunch or evening meal. But if you take other medicines at this time then talk to your prescribing team about how to schedule these medicines
- Constipation is the main side effect, and the dose should be increased slowly, to avoid this. If constipation does not improve, contact your prescribing team.
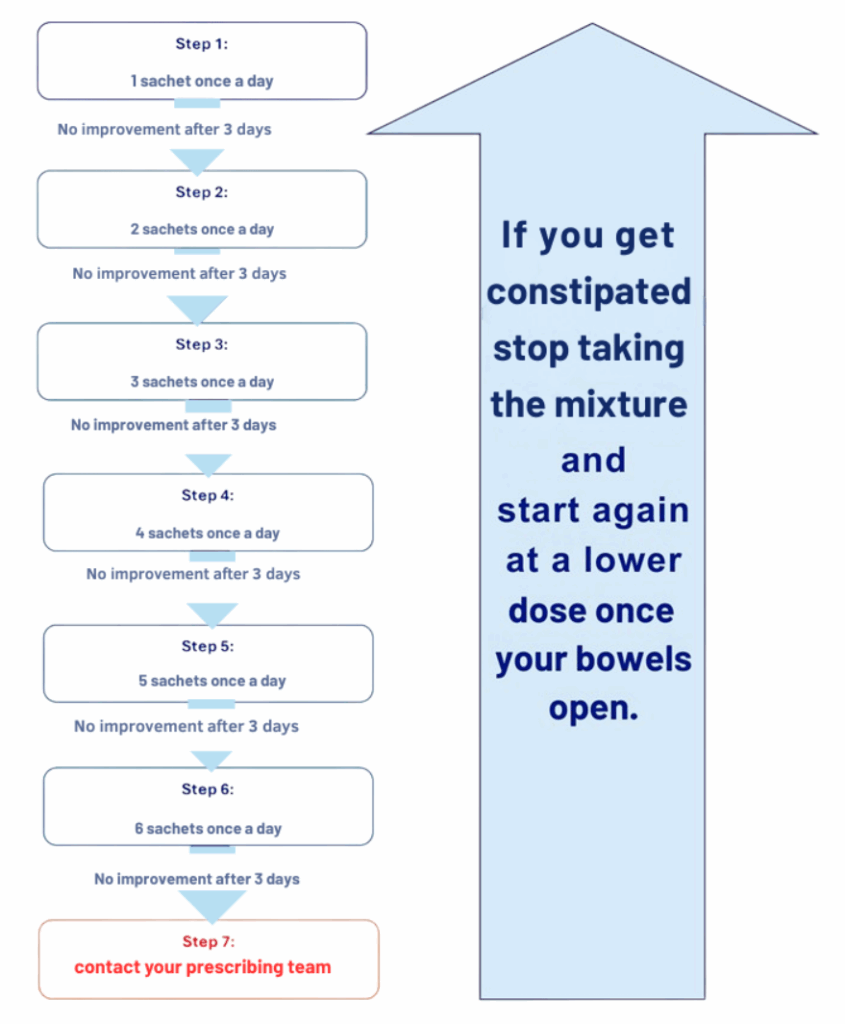
- Colestyramine (powder)
- Start with a low dose and increase slowly to avoid constipation (see flow chart)
- The sachets must be mixed with liquid before taking
- To improve the taste, you can:
- Blended into juice, smoothies, sauces, or desserts
- Put the mixture in the refrigerator
- It is advised that you take it as a single daily dose and take it at least one hour before, or four hours after other medicines
- Works well if taken at lunch or evening meal. But if you take other medicines at this time then talk to your prescribing team about how to schedule these medicines
- Constipation is the main side effect, and the dose should be increased slowly, to avoid this. If constipation does not improve, contact your prescribing team.
Are there any risks with these medicines?
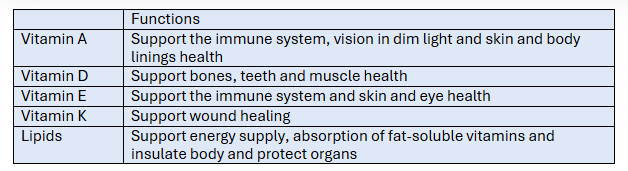
Yes. Bile acid sequestrants can reduce the absorption of fat-soluble vitamins (A, D, E, and K) and fats (lipids). This can reduce important body functions.
If you take these medicines regularly, we recommend:
- Taking a multivitamin and possibly a vitamin D supplement
- Having your vitamin and lipid levels checked at 3 months, and then yearly
Can I use other diarrhoea medicines?
Yes. Medicines such as loperamide can help slow bowel activity and ease diarrhoea. Some people find these work just as well as bile acid sequestrants, and they can be used alone or together. If needing more loperamide than the package recommendations, please speak to your GP.
Where can I find more help?
- Reliable resources:
- Guts Charity Guts Charity
- NHS Choices NHS Choices
- NICE guidelines NICE
- Nutrition UK Nutrition UK
Contact details
Your GP (local contact details)
UHSussex (RSCH/PRH) Digestive Diseases team
ask for Digestive Diseases secretaries office
01273 696955
This leaflet is intended for patients receiving care in Brighton and Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Today’s research is tomorrow’s treatments. That’s why UHSx is proud to be a research-active Trust. Find out how you can get involved.
Visit our website www.uhsussex.nhs.uk/research-and-innovation/information-for-patients-and-public or scan the QR code: