Download and print as a PDF (429kB pdf)
On this page
What does a healthy kidney do?
People normally have two kidneys which lie under the ribs at the back, just above the waist as shown in the diagram below.
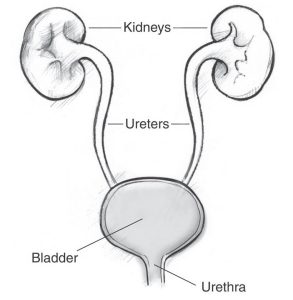
- The main function of healthy kidneys is to filter your blood which passes through the kidneys several times a day. The body’s waste products along with the excess fluid are removed from the blood and the kidneys produce urine to get rid of them. Urine passes from the kidneys down the ureters to the bladder and out through the urethra.
- The kidneys control the amount of water in the body which helps to control blood pressure and prevents the legs swelling or water getting on the lungs and making you breathless.
- Healthy kidneys also produce hormones which control blood pressure and prevent anaemia.
- Healthy kidneys balance many important chemicals in the blood and maintain healthy bones
What is chronic kidney disease?
Chronic kidney disease (CKD) is a long-term condition where the kidneys slowly stop working. This means the kidneys are not able to do their usual jobs, such as removing excess water and waste from the body. As a result, harmful toxins and excess fluid build up in the body.
Usually people with CKD have kidneys that are damaged permanently and their damaged kidneys may stop working altogether as the disease progresses. The speed at which CKD gets worse varies from person to person. It can be slowed down with medication and lifestyle changes but once the kidneys have started failing, they usually get worse.
Classification of Chronic Kidney Disease
The table below shows the different stages of Chronic Kidney Disease (CKD).
| CKD Stage | GFR (ml / min / 1.73m2) | Description |
|---|---|---|
| 1 | >90 | Normal renal function but evidence of kidney damage |
| 2 | 60-89 | Mild reduction in renal function with other evidence of kidney damage |
| 3A | 45-59 | Moderately reduced renal function |
| 3B | 30-44 | Moderately reduced renal function |
| 4 | 15-29 | Severely reduced renal function |
| 5 | <15 | Established kidney failure or end stage renal failure |
What causes kidney disease?
There are many known causes of kidney diseases. These include:
- Inflammation of the kidney (glomerulonephritis) which progressively damages the filtering units (‘glomeruli’ and ‘nephrons’) in the kidneys
- Reflux nephropathy (when urine flows backwards into the kidneys)
- Diabetes
- Genetic (inherited) problems such as polycystic kidney disease (PKD)
- Long term use of pain killers such as non-steroidal, anti-inflammatory drugs (for example ibuprofen) and some other drugs
- High Blood pressure (hypertension)
- Autoimmune disorders (when the immune system attacks the kidney as if it were foreign tissue)
- Blockages of the kidneys, such as kidney stones.
- Previous undiagnosed obstruction to the bladder (e.g. prostate enlargement in men)
- Disease that requires the removal of kidneys, such as kidney cancer.
- Structural defect which means the kidneys do not develop properly in an unborn baby.
What happens when the kidneys fail?
If the kidneys are damaged, they may carry on producing urine but becomes less efficient at removing waste products and fluid from the blood. Instead, the waste products continue to circulate and build up in the blood stream. Damaged kidneys are also less able to remove certain medicines from the body, and these may cause side effects if the drug doses are not reduced. At the same time the production of the hormone ‘erythropoietin’ in the kidneys may be reduced. This can result in production of fewer red blood cells which can cause anaemia.
What are the symptoms of kidney failure?
For many patients the development of kidney failure is a gradual process and until severe may cause you no symptoms. Over time however, it can cause a wide range of symptoms:
- Generally feeling ill; lacking interest in everyday activities; difficulty in concentrating
- Tiredness and loss of energy
- Shortness of breath (due to the build up of fluid in the body and lungs)
- Passing urine more frequently at night
- Feeling sick (nausea)
- High blood pressure
- Loss of libido/sex drive
- Depression
- Altered taste or appetite
- Other symptoms may include cramps, itching and swelling of the legs.
Not everyone will experience all these symptoms which may develop over a period of time varying from months to years.
It can be such a gradual process, some people don’t even realise their symptoms are due to kidney disease until with treatment they begin to feel better.
Regular blood tests will help determine when treatment of kidney failure needs to begin. This may not be for months, or years or you may need to start as soon as possible. It depends on a number of factors such as your general health, the degree of your kidney failure, and how rapidly it is getting worse.
Coping with chronic kidney disease
People with chronic kidney disease can lead full lives but they often need to make changes so that they can manage their disease. Many people with CKD need help from other people, especially if it progresses to established kidney failure. This help can come from their family, friends and/or health professionals.
People choose to cope with their illness in different ways. Being active in choosing treatment and in managing the illness helps maintain a feeling of being in control and helps people make sure they get the treatment that best suits their lives. People with CKD who become more involved in the management of their care have better health outcomes.
Diet
The kidney helps to eliminate waste products from the body. As your kidney function gets worse the kidneys are not able to remove all these waste product such as potassium, phosphate
and salt; and these will start to accumulate in the blood. During this time you will be asked to make changes to your diet. We will make these changes based on the results of your blood test. You will be referred to the renal dietician as necessary, and they will support you to make these changes. Over time you will find that advice
and changes to your diet may appear contradictory. This is because diet adjustments are constantly made according to each blood test. You can also contact the dieticians on 01273 064327 or email them on [email protected].
Healthy living
People with CKD are at risk of developing other complications such as increased cholesterol, high blood pressure if they do not
live a healthy lifestyle. However you feel, it is wise to keep up regular and gentle exercise (passive or active) such as walking, cycling, dancing or swimming if you are able.
If you are in a wheel chair, arm and leg exercises will help to keep you feeling well. You can also read our renal failure and exercise booklet for more information.
Eating food low in fat (as shown in the picture), sugar and salt will also keep you healthy.
If you need any support in maintaining healthy living please ask a member of staff or ring the renal dieticians.
Vaccinations
When your kidney function is low we will advise you to have the following vaccinations against:
- Pneumonia – every 5 years
- Hepatitis B – course of three to four vaccinations, boosters are required
- Flu– every year.
Medicines
As your kidney disease becomes more advanced, various tasks which are usually carried out by the kidneys are lost. In some cases medication is able to replace some of the tasks and in others it may be required to control the symptoms of kidney failure.
By the time you need dialysis, you are likely to be on a number of medications which will be tailored to you individually. When buying over the counter and homeopathic remedies please state that you have reduced kidney function.
Medications to avoid
Non-steroidal and anti-inflammatory drugs (NSAIDs) such as ibuprofen, diclofenac and naproxen or medications containing them.
Antibiotics for urine infections: Avoid trimethoprim and nitrofurantoin.
On the back of your green prescription, there is a list of different categories that can entitle you to obtain your prescription items free of charge. One of these categories is a medical exemption certificate, which in certain circumstances may be issued to you by your health care professional. If you do not fall into any of the categories listed, you will need to pay the current prescription charge or obtain a pre-payment certificate. If you have any concerns about your medications at any time please talk to a member of the renal team or call the renal pharmacist on 01273 696955 Ext. 67586.
Is counselling available?
Dealing with chronic kidney disease and the transition to starting renal replacement therapies such as dialysis can be difficult. People go through a range of emotions as they adjust to the new lifestyle. We have specialist renal counsellors who can help you to discuss these feelings. To speak to a counsellor please call 01273 064097.
Financial support
Advice regarding financial and social support is also available. We have a separate information leaflet on financial and social support. For assistance with benefits applications, housing issues and information about the range of support services available to you please contact our welfare advisor on 01273 696955 Ext. 67886.
Questions frequently asked
Useful websites
- Edinburgh Renal Unit
- Kidney Patient Guide
- NICE Guidelines
- NHS Chronic Kidney Disease
- NHS Kidney care
- Kidney Care UK (previously known as British Kidney Patients Association) Telephone: 01420 541424
- National Kidney Federation Telephone: 0800 1690936 (Freephone)
- Kidney Research UK.
- Nephron information centre
- Buckfield Dialysis
- NHS Kidney care resources
- Kidney unit
Contacts
Please talk to staff at the kidney unit if you have any questions.
Outside normal working hours you can contact staff on the renal ward.
You can write to us using the address below:
Sussex Kidney Unit
Brighton and Sussex University Hospitals NHS Trust
Royal Sussex County Hospital
Eastern Road, Brighton BN2 5BE
Renal Outpatient Department
01273 664559
Main Dialysis Unit
01273 696955
Ext. 64605
Renal Ward
01273 696955
Ext. 64037
Home care therapies
01273 696955
Ext. 64558
Worthing Satellite
01903 285244
Crawley Satellite
01293 511776
Bexhill Satellite
01424 731824
Polegate Satellite
01323 489158
The information here is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.