Download and print as a PDF (225kB pdf)
On this page
- Why have I been given this information?
- Why do I have to have a biopsy?
- What is Giant Cell Arteritis?
- What symptoms or signs do people with GCA often have?
- What might happen if I have changes in my vision and treatment isnât started quickly?
- What do we do to help you if we think you may have GCA?
- What will happen just before the biopsy, when Iâm having it and when Iâm ready to go home?
- What are the risks of having the biopsy done?
- Will the results of the biopsy always show whether I have GCA?
- Why might I have a false negative result?
- What happens if you think I may have a false negative result?
- Frequently Asked Questions
- Who can I contact if Iâd like more information about my treatment?
Why have I been given this information?
You have been referred to the Maxillofacial Unit (MFU) for a temporal artery biopsy (TAB).
Why do I have to have a biopsy?
You are having a TAB because we think you may have a condition called Giant Cell Arteritis (GCA). A biopsy will help us to make a diagnosis.
What is Giant Cell Arteritis?
Giant Cell Arteritis (GCA) is inflammation of the blood vessels.
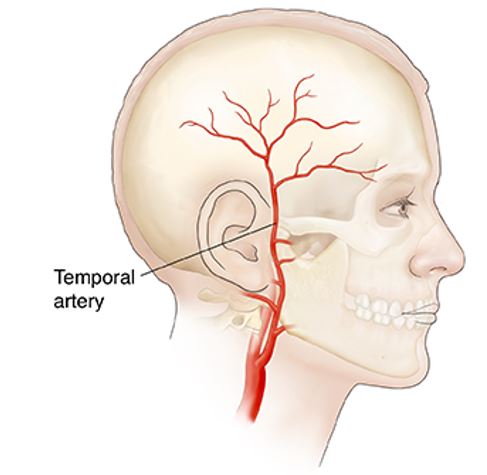
It mostly happens in the head (sometimes called ‘temporal arteritis’) but it can happen in any medium to large sized arteries in the body.
Many people with GCA also have a condition called Polymyalgia Rheumatica (PMR) which causes pain and stiffness in the neck, upper arms, shoulders and hips.
What symptoms or signs do people with GCA often have?
People with GCA often have some of these signs and symptoms:
- New throbbing headache on one side of your head or back of the head
- Tenderness when you touch your scalp
- Pain or an uncomfortable feeling in your jaw, especially when chewing (Claudication)
- Blood vessels at the side of your forehead that look like they’re bulging or sticking out from the forehead
- Tiredness, not feeling hungry, losing weight
- Changes in your vision including:
- blurred vision
- seeing double
- suddenly not being able to see (blindness in one or both of your eyes)
What might happen if I have changes in my vision and treatment isn’t started quickly?
Permanent damage to your sight can happen if treatment isn’t started quickly.
What do we do to help you if we think you may have GCA?
- If we think you may have GCA we will always start by giving you a high dose of a type of medicine called steroids which help to reduce inflammation. After you’ve had your biopsy we’ll decide if you still need the steroids. If you do need to stop taking this medicine, it’s important that you do this gradually, so we’ll reduce the dose or get you to take it less often.
- Your doctor will often take a set of blood tests to include ESR (erythrocyte sedimentation rate) and CRP (C-reactive protein) which are signs of inflammation. These are almost always raised if you have GCA.
- If you have eye symptoms your doctor will also refer you to an eye specialist (Ophthalmologist)
- The jaw and face doctors (Maxillofacial) team will offer you a biopsy to help with your diagnosis so your GP or specialist can look after you in the best way.
- We will usually do the biopsy within two weeks of starting steroid treatment.
What will happen just before the biopsy, when I’m having it and when I’m ready to go home?
- You should have something to eat and drink before you come for your biopsy.
- The appointment takes approximately 45 minutes. This includes:
- meeting the surgical team
- explaining the procedure
- answering any questions you may have
- getting your consent using a consent form
- doing the biopsy
- We use a small jelly scan (Doppler machine) to map out the artery and decide where to take the sample from.
- Sometimes we will need to shave off a small amount of hair if it lies over the place where the biopsy will be taken from.
- The biopsy will be done under local anaesthetic (you are awake, the same as being at the dentist). You will be given some local pain-killing (anaesthetic) injections to numb the area where the biopsy will be taken from so you won’t feel any pain.
- Once you’re comfortable, a small cut will be made in your skin to get to the artery and a sample taken. This sample is sent to a pathologist to examine under the microscope. The results are sent to your GP and they will contact you to tell you what the biopsy shows.
- Your skin will be stitched back together, usually with dissolving stitches that do not need to be removed.
- You will be given a leaflet which will tell you how to look after yourself and who to contact if you need help after your biopsy.
- When we’ve discharged you, you’ll be able to go home.
What are the risks of having the biopsy done?
Common side effects include:
- a small amount of bleeding or oozing from the wound
- bruising
- discomfort or tenderness
- swelling
- infection
- a small line of scarring, often in the hairline
Rare side effects include:
- bleeding from the artery from where the biopsy was taken or having heavier bleeding
- numbness of the skin around the cut. This might go away soon but it might never go away
- weakness of the eyebrow. This might go away soon but it might never go away
Will the results of the biopsy always show whether I have GCA?
No. Some biopsies don’t give a full or accurate result. This is called a non-diagnostic biopsy.
You might still have GCA even if the results of your test make us believe that you don’t. This is called a ‘false negative result’.
Why might I have a false negative result?
This can happen if you have been on steroid treatment for a while before the biopsy is done. It can also happen if we take the biopsy from a part of the artery that the GCA hasn’t damaged very much.
What happens if you think I may have a false negative result?
You will already be on the best treatment for GCA (steroids) so you won’t have another biopsy. Your GP or inflammatory diseases specialist (Rheumatologist) will monitor your condition and gradually reduce your dose of steroids until you don’t need to take them anymore.
Frequently Asked Questions
I’m taking medicine to thin my blood. Do I need to stop taking it before I have the TAB?
Yes. If you’re taking Warfarin stop taking it three days before your biopsy. If you’re taking apixaban, rivaroxaban or dabigatran (NOACs) stop taking them two days before your biopsy.
If you’ve ever had a blood clot in the past (DVT/pulmonary embolism/stroke) or have any questions or worries about your blood thinner please ask your GP.
If GCA can affect any artery, why do you take a biopsy from the side of the forehead (temple) area?
These arteries are the ones that are most often affected if you have GCA and they’re only just under the skin so are easy to take the biopsy sample from.
The path of the artery means we can often hide the scar in the hairline.
Will having the TAB affect the blood supply to my head if you take a piece of my temporal artery?
No. There are many blood vessels taking blood to the head and neck so the blood supply will still be enough if we take a small piece of this artery.
We tie the end of the artery off once the sample has been taken to stop any bleeding.
Should I be worried if you’re uncertain whether I have GCA or not after my biopsy?
No. Whether a diagnosis can be made or not, please be reassured your treatment path is correct.
Who can I contact if I’d like more information about my treatment?
If you have any questions about your treatment or would like more information, please see our web page or contact your local Maxillofacial Unit:
Maxillofacial service web pageMaxillofacial Unit St. Richard's Hospital
St. Richard’s Hospital, Spitalfield Lane, Chichester, PO19 6SE
Phone
01243788122
Ext. 33322
Maxillofacial Unit Worthing Hospital
Worthing Hospital, Park Avenue, Worthing, BN11 2DH.
Phone
01903205111
Ext. 84067
We are committed to making our publications as accessible as possible. If you need this document in an alternative format, for example, large print, Braille or a language other than English, please contact the Communications Office:
email: [email protected]
or speak to a member of the Maxillofacial unit.
This leaflet is intended for patients receiving care in St. Richard’s Hospital, Chichester and Worthing Hospital. The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.