Download and print as a PDF (888kB pdf)
On this page
- What is the Enhanced Recovery Programme?
- How can you help us before you come in for your surgery?
- What will happen in the Pre-Assessment Clinic?
- What should I bring into hospital?
- What can I eat and drink before my operation?
- What about my usual medicines?
- What about infection control?
- What can I expect after my surgery?
- Why are exercises an important part of my recovery?
- What should I do if I have concerns after I leave hospital?
- Will I need a follow up appointment?
- What is my âDaily Diaryâ?
- Your daily diary
- Further notes
- References/useful links
What is the Enhanced Recovery Programme?
The aim of the Enhanced Recovery Programme (ERP) is to get you back to full health as quickly as possible after your operation. Research indicates that after surgery, the earlier you get out of bed and start eating and drinking the better. This will speed your recovery making it less likely that complications will develop.
For example, the benefits of getting up and about are:
- Returning to eating and drinking much sooner
- Reduced risk of chest infection
- Less muscle wasting, so that function and mobility are maintained
- Less tiredness
- Reduced risk of developing blood clots
To achieve this, however, we need you to be a partner with us so that we can work together to speed your recovery. This leaflet will increase your understanding of the programme and ensure you play an active role in the preparation for your operation and your recovery. Before you come into hospital your gynaecologist will see you and explain the programme to you, where you will be given the opportunity to ask questions.
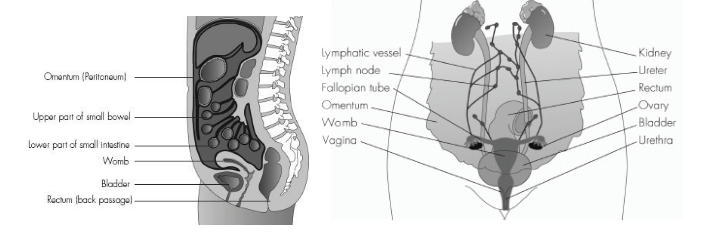
Below is a picture of your female anatomy. Your gynaecologist will show which part of you is to be removed.
Name of planned operation:________________________________________________________
How can you help us before you come in for your surgery?
If you optimise your health in the weeks before your operation then you will recover more quickly and have fewer complications. Try to eat as healthily as possible and you may consider taking a multivitamin and mineral supplement every day to make sure you have a good level of essential nutrients. Do not diet in the weeks before an operation but also avoid putting on a lot of weight. Ensure adequate exercise and walk whenever you can.
Also, think about how you can cope in the weeks after surgery when you are recovering. Can you arrange help from family or friends? If you think that you will have problems at home after your operation then seek help early so a suitable solution can be found before your operation. Make sure that you raise any concerns that you have in the pre-assessment clinic.
If you are a smoker it is advisable for you to stop. Smokers are more prone to complications and chest infections after surgery. You may wish to contact a local helpline on 01273 267397 or if you have access to the internet log on to www.nhs.uk/smokefree for help and advice in quitting smoking.
If you are diabetic or you are taking tablets for your heart or lungs, you should make an early appointment with your GP so that they can make sure you are taking the right medication before surgery. Show them this booklet to let them know that the hospital has advised you to do this.
What will happen in the Pre-Assessment Clinic?
1 to 2 weeks before your admission date you will be seen in the pre-assessment clinic. The clinic is run by experienced nurses. The purpose of the clinic is to assess your fitness for a general anesthetic and provide you with specific information about your admission. This ensures that your operation and hospital stay goes as smoothly as possible. This will be an opportunity for you to ask questions and tell us about your individual needs and circumstances. It is important for you to tell us as early as possible if you have any concerns about whether you will be able to manage your daily activities after you leave hospital. We will help you make the necessary arrangements.
Please bring with you any medicines that you usually take and also contact numbers for your next of kin as we will make a record of both of these things and then return them to you.
If you have been told that you may require a stoma (ileostomy or colostomy) to be formed as part of your surgery, you will be referred to one of our specialist stoma care nurses prior to your admission for support and information. The nurse will then see you before your operation to mark a suitable site on your abdomen and will provide ongoing support and education. On the day after your operation you will be encouraged to begin to participate in learning to care for your stoma. You will not be sent home until you can manage your stoma by yourself so learn about stomas and ask questions as soon as you can if you are told that you might have one.
If you have any concerns about your date of operation please contact the gynaecology admissions department.
What should I bring into hospital?
Always bring this booklet with you whenever you visit the hospital from now until your first follow-up clinic appointment after your operation.
We suggest you bring in:
- Toilet bag with wash things
- Sanitary Towels
- Box of tissues
- Loose-fitting night clothes
- Dressing gown and slippers (Please ensure that your slippers are well fitting and if they are not please bring in shoes instead)
- Maybe a book or magazines
- A small amount of money for Patientline (hospital TV, telephone and radio). The Patientline cards cost £5 or £10 and can be purchased from the vending machine on the ward, or via debit/credit card over the telephone. Once registered the radio is free
When you come to stay in hospital for your operation, do not bring in anything of potential value e.g. jewellery, credit cards etc. Please keep your property to a minimum, as there is limited space in your locker.
Please arrange for friends/relatives to take bulky items such as bags/suitcases home as soon as possible for access to clean around your bed area and due to limited storage space. Please do not send your outdoor clothes home as you will need them the morning of your discharge.
What can I eat and drink before my operation?
You can have clear fluids 2 hours prior to your admission or until 6:30am and then you will need to fast (be Nil by Mouth).
| Admission Time | No food from | Clear fluids until |
| 07.30 | 02.30 | 06.30 |
| 08.00 | 02.30 | 06.30 |
| 08.30 | 02.30 | 06.30 |
| 10.30 | 04.30 | 08.30 |
| 11.00 | 05.00 | 09.00 |
| 12.00 | 06.00 | 10.00 |
If you are having abdominal surgery (a cut in your tummy) a key aspect of the enhanced recovery programme is that you will consume a carbohydrate based nutritional drink before your surgery. The benefit of this is that it will give you much needed energy to help you recover.
You must drink 250mls of an isotonic solution such as non fizzy Lucozade Sport (500mls) the evening before your surgery. The remaining 250 mls should be drunk the morning of surgery, two hours prior to fasting.
Your gynaecologist will decide whether you require bowel preparation to clear the contents of your bowel out prior to surgery. This will involve having an enema the morning of your surgery before you go to theatre.
What about my usual medicines?
Please bring into hospital any medication that you usually take on prescription in their original boxes. The doctor in pre-assessment will tell you which of these should be taken before and on the day of your surgery.
You will be given a pair of surgical stockings to wear which reduce the risk of blood clots forming in your leg veins. You will also be given a daily injection of a blood thinning drug post-operatively and on discharge. The nurses will teach you or a relative how to do these injections in preparation for home.
What about infection control?
Hand hygiene is the best way to prevent germs spreading. To help reduce the risk of getting an infection in hospital, please read the following advice:
- Keep your hands and body clean
- Always wash your hands after using the toilet
- If you are using a commode ask for a moist wipe afterwards
- Always wash your hands or use a moist wipe before you eat your meal
- If a member of staff needs to examine you or perform a procedure, do not be afraid to ask if they have first washed their hands or used a hygienic hand rub. Staff should wear a plastic apron and gloves for procedures such as taking blood, undertaking dressings etc.
- Keep your locker and bedside table tidy and free from clutter and ensure none of your possessions are on the floor. This will make it easier for staff to clean properly
- Ask your visitors to use the hand gel provided on entering and leaving the ward
- Please remember flowers are not permitted throughout the hospital
It may feel awkward to question staff when someone is looking after you, but you are entitled to ask/remind health care staff to wash their hands.
MRSA stands for Methicillin Resistant Staphylococcus Aureus. This is a form of Staphylococcus Aureus (SA). SA is the commonest type of bacteria which can infect humans. About a third of the population are colonised with SA. Colonised means the organism lives harmlessly on skin or in the nose. SA causes problems when it enters the body and this is most likely when patients are unwell. MRSA is a variety of SA that tends to spread easily.
Before you come into hospital for your operation, you will have a pre assessment appointment. During this appointment two painless swabs will be taken, one from inside the nose and one from the perineum (which is the area between the vagina and the anus). These are the areas of the body where MRSA is most likely to be found in carriers. If you are unable to do your own perineum swabs a nurse will assist you.
The swabs will be sent to the hospital laboratory to see if the MRSA germ is present – it can take up to five days to get the results. If your swabs come back positive we will inform you straight away and let you know what treatment is needed. For example, if your nasal swab is positive you will need to use an antibacterial ointment which is applied to your nostrils three times a day for five days. If you have any questions with regard to infection control, please speak to your nurse.
What can I expect after my surgery?
After your operation you will be transferred to the recovery area of theatres where you will stay until you are awake, comfortable and stable. Your nurse will then come and transfer you to the gynaecology ward. Occasionally your doctors may feel a different ward is more appropriate for you after your surgery and this will be explained to you if necessary.
You will be given a leaflet specific to your surgery that will tell you what to expect post-operatively and will advice you on ‘dos and don’ts’.
Why are exercises an important part of my recovery?
The quicker you begin to start moving around, the quicker you may leave hospital. Your recovery starts immediately after your surgery and you will be encouraged to start your breathing exercises as soon as you wake up.

On the day following your surgery the nurses will help you to sit out of bed, it is advised that you sit out three times; you can link this with meals as it will aid digestion. A nurse will accompany you to mobilise until you are judged safe to do so on your own. If you require mobility aids or need to practice the stairs then this can be arranged.
Most patients can conduct their own physiotherapy exercises after their operation and these are described below for you. Deep breathing and limb exercises are known to strengthen and enhance recovery after surgery. At the very least you should take a deep breath in and move all limbs every waking hour after your operation. Try these exercises out before your operation.
Other simple exercises
The more active you can be the quicker you can recover from your surgery and prevent complications.

You can march or kick out your legs, tap your toes and reach up with your arms to optimise your circulation and muscle strength after your surgery.
Breathing exercises
Due to the effects of the anaesthetic and some of the pain relief you may have been given you may not breathe as deeply as you would normally. This could result in less oxygen circulating in your body. Oxygen is essential for healing tissues. After your surgery you may have pain and be reluctant to move around, take a deep breath or cough forcefully. However, this is important to keep your lungs healthy and prevent infection so your nurse will show you techniques to breathe effectively and clear your chest comfortably. You will also be encouraged to start moving around more as this is the best way of keeping your lungs healthy and optimising your circulating oxygen.
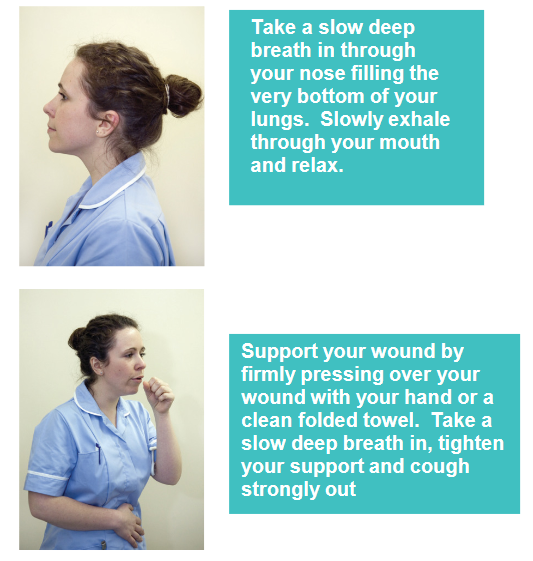
Deep breathing exercises increase the volume of air in your lungs and help you cough up any phlegm. A supported cough will comfortably help to clear your lungs. You should try to do 3 of these exercises every couple of hours to ensure your lungs are working as well as possible.
What should I do if I have concerns after I leave hospital?
Complications do not happen very often. However it is important that you know what to look out for. If you are worried during the first 4 weeks after surgery then please contact us:
Royal Sussex County Hospital
Level 11
01273 696955
Ext. 64013 or 64022
Princess Royal Hospital
Horsted Keynes
01444 441881
Ext. 65685 or 65686
A nurse from the gynaecology ward will telephone you at home on the first and second days following your discharge to see how you are progressing and answer any questions you may have. If after 4 weeks you experience any problems please contact your GP.
Abdominal pain
If you have severe pain lasting for more than two hours or have a fever and feel generally unwell please contact us and we will advise you.
Vaginal Discharge/Bleeding
You can expect to have some vaginal discharge/bleeding for 1–2 weeks after surgery. This is like a light period and is red or brown in colour. Some women have no bleeding initially and have a sudden gush after about 10 days; this is quite normal and should settle quickly. Sanitary towels should be used, not tampons, to reduce the risk of infection. If you experience any heavy bleeding and you’re concerned please contact us.
Your wound
It is not unusual for your wounds to be slightly red and uncomfortable during the first one or two weeks. Please let us know by telephone if your wounds become inflamed, painful or swollen or start to discharge fluid.
Your bowels
Your bowel habits may change temporarily. Your motions may become constipated or may become loose. Make sure you eat regular meals 3 or more times a day, replace any fluid lost and take regular walks. In most patients their bowels settle down a few weeks after surgery. However, you may not go completely back to the usual bowel habit you had prior to your operation.
Passing urine
Sometimes after gynaecological surgery you may experience a feeling that your bladder is not emptying fully. This usually improves with time. If it does not improve or you have excessive stinging when passing urine, you must make an appointment to see your GP. Take a sample of urine with you or be prepared to give a sample if asked to at your appointment.
Will I need a follow up appointment?
For most patients a follow up appointment is not necessary, your gynaecologist will inform you before you leave hospital if they feel they need to see you again. For some patients it may be necessary to send samples/specimens from your operation to the laboratory for testing. Your gynaecologist will inform you if they have done this and will offer either an appointment or telephone call to receive histology results, this is usually within 3 weeks of your operation. They will inform you whether or not any further treatment will be recommended.
If you do need an appointment or you are expecting a telephone appointment make sure that you write down any questions or concerns that you might have on a piece of paper because it can be very frustrating if important questions are forgotten when you speak to the doctor. After your operation your gynaecologist will write a letter about you to your GP so that they can continue with your medical care in the community.
What is my ‘Daily Diary’?
On the following pages we have written a diary that we want you to complete on the first few days after your operation. This will help guide you and hopefully get you more involved with striving to ensure a good recovery.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Your daily diary
Each day please complete your personal activity plan. If you didn’t achieve an activity there is space for you to document why not and also for other thoughts etc. that you may wish to write down.
Your first day after surgery. Date:_____________________________
| Have you? | Tick |
| Done your deep breathing exercises every waking hour | |
| Done your limb exercises every waking hour | |
| Changed your position at least every two hours to include lying tilted on your side to ensure you have relieved the pressure on your bottom | |
| Told the nurse if you have pain or nausea | |
| Sat out of bed in the morning for two hours | |
| Sat out of bed in the afternoon for two hours | |
| Sat out of bed in the evening for two hours | |
| Walked at least 60m with the nurse this morning | |
| Walked at least 60m with the nurse this afternoon | |
| Walked at least 60m with the nurse this evening | |
| Discussed your discharge plans with the nurse | |
| Made transport arrangements for getting home | |
| Eaten breakfast | |
| Eaten lunch | |
| Eaten supper | |
| Eaten some snacks between meals | |
| What has been your pain level today? Please indicate: 0 (no pain) 1 2 3 4 5 (moderate pain) 6 7 8 9 10 (excruciating pain) |
Comments and questions:
_________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
Day 2 Date:_______________
| Have you? | Tick |
| Done your deep breathing exercises every waking hour | |
| Done your limb exercises every waking hour | |
| Changed your position at least every two hours to include lying tilted on your side to ensure you have relieved the pressure on your bottom | |
| Told the nurse if you have pain or nausea | |
| Sat out of bed in the morning for two hours | |
| Sat out of bed in the afternoon for two hours | |
| Sat out of bed in the evening for two hours | |
| Walked at least 60m with the nurse this morning | |
| Walked at least 60m with the nurse this afternoon | |
| Walked at least 60m with the nurse this evening | |
| Discussed your discharge plans with the nurse | |
| Eaten breakfast | |
| Eaten lunch | |
| Eaten supper | |
| Eaten some snacks between meals |
Comments and questions:
_________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
Day 3 Date:_____________________
| Have you? | Tick |
| Done your deep breathing exercises every waking hour | |
| Done your limb exercises every waking hour | |
| Changed your position at least every two hours to include lying tilted on your side to ensure you have relieved the pressure on your bottom | |
| Told the nurse if you have pain or nausea | |
| Sat out of bed in the morning for two hours | |
| Sat out of bed in the afternoon for two hours | |
| Sat out of bed in the evening for two hours | |
| Walked at least 60m with the nurse this morning | |
| Walked at least 60m with the nurse this afternoon | |
| Walked at least 60m with the nurse this evening | |
| Discussed your discharge plans with the nurse | |
| Eaten breakfast | |
| Eaten lunch | |
| Eaten supper | |
| Eaten some snacks between meals |
Comments and questions:
_________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
Day 4 Date:________________________
| Have you? | Tick |
| Done your deep breathing exercises every waking hour | |
| Done your limb exercises every waking hour | |
| Changed your position at least every two hours to include lying tilted on your side to ensure you have relieved the pressure on your bottom | |
| Told the nurse if you have pain or nausea | |
| Sat out of bed in the morning for two hours | |
| Sat out of bed in the afternoon for two hours | |
| Sat out of bed in the evening for two hours | |
| Walked at least 60m with the nurse this morning | |
| Walked at least 60m with the nurse this afternoon | |
| Walked at least 60m with the nurse this evening | |
| Discussed your discharge plans with the nurse | |
| Eaten breakfast | |
| Eaten lunch | |
| Eaten supper | |
| Eaten some snacks between meals |
Comments and questions:
_________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
Day 5 Date:__________________________
| Have you? | Tick |
| Done your deep breathing exercises every waking hour | |
| Done your limb exercises every waking hour | |
| Changed your position at least every two hours to include lying tilted on your side to ensure you have relieved the pressure on your bottom | |
| Told the nurse if you have pain or nausea | |
| Sat out of bed in the morning for two hours | |
| Sat out of bed in the afternoon for two hours | |
| Sat out of bed in the evening for two hours | |
| Walked at least 60m with the nurse this morning | |
| Walked at least 60m with the nurse this afternoon | |
| Walked at least 60m with the nurse this evening | |
| Discussed your discharge plans with the nurse | |
| Eaten breakfast | |
| Eaten lunch | |
| Eaten supper | |
| Eaten some snacks between meals |
Comments and questions:
_________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
Further notes
Add anything here that you want to ask your nurse on the telephone call follow up after discharge from the hospital or that you want to ask the doctor.
________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
Please help us to improve our care for future patients. If you found something particularly helpful or particularly unhelpful or difficult during your patient journey on the Enhanced Recovery Programme then it would be much appreciated if you could let us know by writing to:
The Ward Sister
Level 11 Ward
Tower block
Royal Sussex County Hospital
Eastern Road
Brighton
East Sussex
BN2 5BE
Thank you.
References/useful links
1. NHS National Institute for Innovation and Improvement (2008). Enhanced Recovery Programme.
2. NHS Improvement (2011) Enhanced Recovery
3. Department of Health (2010) Enhanced Recovery
This information is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information here is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.