Print and download as a PDF (614kB pdf)
On this page
- Introduction
- How you can help before your surgery
- Upper limb exercises to practice
- Stress
- The way we feel when we are stressed is caused by 3 overlapping features:
- My personal plan
- Discharge arrangements
- Before your admission
- To do list
- Patient diary
- Hospital admission
- To further aid your recovery whilst at home
- What to do if you have concerns after you have left hospital
Introduction
The aim of the Enhanced Recovery after Surgery (ERAS) programme is for you to return to full health as soon as possible after your operation. Research has shown that the earlier you get out of bed and start eating and drinking the quicker your recovery.
The programme will begin before your operation, progress through your care whilst in hospital and continue when you are back at home.
There are many ways you can speed up your recovery. This booklet will increase your understanding of the ERAS programme and enable you to take an active role in your preparation for surgery and your recovery after.
Please do also read through your patient information booklet regularly as this contains all the information regarding all aspects of your cardiac surgery journey.
Thank you for attending your pre-assessment appointment today with:
- Gemma Sowky (Working on Weds, Thurs, Fri)
- Lou Pope (Working on Mon, Tues, Fri)
- Renata Sobral (Working on Mon, Tues, Weds, Thurs).
If possible, please phone the sister that has pre-assessed you on the appropriate days. Our telephone number is 01273 067423 and our email address is [email protected].
We are your point of contact whilst you wait for surgery and we will be helping to get you fit and ready for surgery and organising any further tests you require. Please contact us if your symptoms become more severe or if you get any infection or bleeding issues, have visited your GP or the hospital for another problem, if your medications have changed or if you have any dental issues.
Once we have a slot for your operation, our cardiac admin team will schedule you for surgery. They will organise your admission and call you one week before to let you know the process. Their telephone number is 01273 696955 and extension number 67205.
Please stop the following medications before your operation – please refer to the PDF of this leaflet to view the table.
How you can help before your surgery
Healthy living goals in the weeks before your surgery will aid you to recover quicker and have fewer complications.
More of the goods (think about healthy eating instead of going on a diet):
- Eat plenty of foods high in fibre (beans, lentils, seeds, nuts, wholemeal, fruit and vegetables. Aim to eat at least 5 portions of fruit and vegetables a day
- Protein and iron rich foods such as lentils, beans, chickpeas, tofu, nuts, lean meat, fish, eggs, dried fruit and leafy green vegetables, especially kale and broccoli
- Wholegrain varieties of starchy foods such as brown rice and brown pasta instead of plain white
- If you’re diabetic follow a strict diabetic diet prior to the surgery to optimise your blood sugars and minimise your infection risk
- Good hydration – drink plenty of water unless you have fluid retention.
Less of the bads:
- Limit fat intake, especially saturated and trans fat that is present in processed and fatty meats like sausages, hamburgers, bacon, butter, margarine and snacks like biscuits, cakes, pies and pastries
- Limit salt intake – less than 2.5g/day
- Limit sugar intake, especially refined sugars – less than 30g/day
- Limit alcohol consumption – alcohol can lead to severe bleeding after surgery, blood and brain complications and wound infections
- Stop smoking 6 weeks before surgery – smoking can lead to chest and wound infections and can also increase bleeding and blood complications after surgery. For help and advice on quitting smoking you may wish to: contact a local helpline on 01273 267397 or online at: Stop Smoking NHS
Stay active
If you feel well enough exercise will help make sure your body is as fit as possible before your surgery. If you are already active, keep up with your normal exercise / activity routine. If not, start slowly adding exercise into your day. A 15 minute walk is better than not exercising at all.
Maintain a healthy weight
Advice will be given if you are found to be underweight or overweight in your pre-assessment clinic appointment.
Get practising
We would like you to start practising the exercises you will be doing after your surgery.
You will have a wound down the centre of your chest over the breastbone. An important part of the wound and bone healing is the restriction of the activities you can do with your arms after your operation. This is because certain activities can put a lot of stress on the bone trying to heal.
The main restriction is no lifting, pushing or pulling with your arms for the first 3 months after your operation. As a guide you should not lift any object that weighs more than 5 lbs (2.2 kgs).
Getting in and out of bed
To make it easier getting out of bed our Physio’s advice is:
- Roll onto either side
- Gently lower your legs off the edge of the bed
- Push down through your elbow and come up into a sitting position
To get into bed the same process is followed in reverse.
Getting in and out of a chair
- Sit on the edge of the chair
- Fold arms across chest
- Feet firmly flat on the floor
- Rock gently backwards and forwards 3 times – on the third rock forward, push up firmly through your legs and come into the standing position.
Upper limb exercises to practice
Straight arm raise
- Stand with hands clasped in front of you and elbows straight
- Lift both arms up over your head and then back down again to the starting position
- Repeat 5 times.
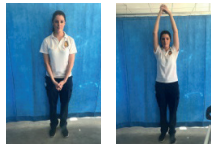
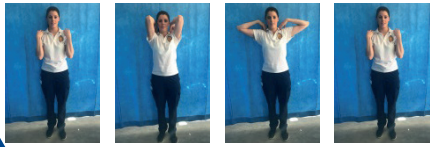
Elbow circles
- Sit or stand
- Place your finger tips on your shoulders
- Lift your elbows up in front of you as high as you can keeping your finger tips on your shoulder
- Bring your elbows out to the side, and then back down to the starting position
- Repeat 5 times.
Stress
Stress is very detrimental for your general health as it releases hormones that can affect how your body systems work and decrease your immune system.
Having cardiac surgery can be a very stressful period because of the following reasons:
- Being in hospital and having medical tests and treatment
- Having operations postponed
- Having to make lifestyle changes such as stopping smoking and changing diet
- Having to learn about and to take new medication
- Feeling at risk of further heart problems
- Troubling thoughts such as “Why did this happen to me?”
- The impact of heart problems on family and friends
- Family and friends being overprotective
- Having to take time off work and then going back to work.
The way we feel when we are stressed is caused by 3 overlapping features:
- The way we think about the situation – Do you focus on the negative aspects which then make you feel down about the situation?
- The way we behave when we are faced with the situation – Do you bottle things up? Are you irritable with family? Do you talk faster than usual?
- The way your body responds in stress – Do you get tense? Do you get headaches? Do you feel restless? Is your heart racing?
When there’s a heart problem, the physical effects of stress can be very confusing and can add to the fear that something is wrong with the heart. That in turn will make you more stressed – a snowball effect.
When we are stressed our body releases hormones, one of which is adrenaline that can make your heart race, cause you to breathe faster, you may sweat, feel tense and have butterflies in your stomach. These symptoms will not harm you, but if they are not addressed they can build up to a point that can be frightening.
10 ways to deal with stress:
- Talk or write – say it to yourself: “I’m feeling stressed” to help you acknowledge your feelings and accept it. You can also share it with someone else to get a new perspective or see it from a different angle. Another way is to write down your worries. It’s easier to see it in perspective when it’s on paper. You can use the patient diary or any other journal/paper.
- Sort it – list practical options, weigh up the fors and againsts and then decide. Establish healthy boundaries.
- Pause and think – then take a fresh look. Is it really so bad? Imagine a few years from now, how important will it be then? Manage your mind chatter focusing on the positive aspects and not giving so much importance to the negative aspects. Our subconscious hears our thoughts and can detect a threat, even if it’s only in our imagination. Don’t believe in everything you think.
- Breathe – breathe in and out slowly a few times. Try to breathe in for a 4 count, hold your breath for a 4 count, breathe out for a 4 count and pause for a 4 count. Repeat 3 to 5 times and see how you feel. When we breathe slowly we are triggering our parasympathetic nervous system, which is the one responsible for rest and relaxation and it gives signals to your body that is time to relax. Relaxation starts in our physical body.
- Move – stand up and move around, do a stretch, go for a walk, especially in nature; as little as 15 minutes can be helpful. If you don’t have access to green spaces nearby, even just looking at pictures of greenery or forest can decrease stress hormones. Shake or dance it out; this is a primal tendency to end a stress cycle like animals would do in the wild. The body is where the stress and anxiety lives but also where it can move and transform.
- Listen to music – relaxing music or just music that you love! Here are some suggestions: Alexis French – Bluebird; Pachelbel Canon in D Major; Marconi Union – Weightless. Organise a dedicated time of your day for relaxation. It’s easier first thing in the morning or last thing at night but anytime that suits your day is the best option. Imagine yourself in a relaxing place and feel what it feels like.
- Declutter – your mind from bad thoughts but also your life from things you don’t need. If you live in a tidy place there’s more chance that you will have a tidy mind.
- Reduce stimulants – coffee, alcohol, sugar. Embrace relaxing drinks like a chamomile, lemon balm or peppermint tea.
- Laugh – look for the funny side. There is one in most situations. Laughter promotes happiness hormones and decreases the sensation of pain.
- Be mindful – be present in this moment, let the past go and don’t constantly worry about the future. Explore the benefits of nature, pets (yours or not) and enjoy life!
My personal plan
Try to see the waiting time as a preparation time for surgery. List down your personal goals to work towards in the meantime while you’re waiting for surgery, i.e. healthy diet, exercise, stop smoking, stop drinking, reduce stress, etc. List them prioritising what you have to do first and then slowly follow your plan through. It might also help to write down strategies to help you to achieve your goals. You will see that once you start achieving one goal you will feel motivated and the other ones will just follow through. Don’t hesitate to call your pre assessment nurse if you need advice or strategies to help you.
Note: please refer to the PDF version of this booklet for the space to write down any thoughts, worries and anything else.
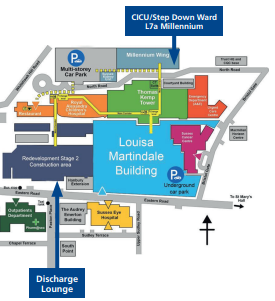
Where to find us
Discharge arrangements
We would like you to start thinking about your discharge before you come into hospital. We routinely use the discharge lounge located in the main entrance of the Barry building.
Once you are medically fit for discharge, we aim to send you to the discharge lounge by midday. From there your family, friend or whoever you have arranged to pick you up can do so easily.
Recovery at home will continue for some time after you are discharged and therefore you need to think about how you will manage in the weeks after surgery.
- make sure you have someone who can collect you from hospital when you are discharged.
- make sure you have someone who can stay with you at home for the first week.
- buy extra shopping of non-perishable foods and ready meals before admission. Arrange for family / friends to get fresh / frozen foods after discharge.
If you think you will have any problems at any stage of your programme, please call and seek help so that appropriate safe solutions can be found in advance.
Before your admission
In the week before your admission we would like you to prepare for your operation by:
- Re-reading your patient information booklet
- Maintaining excellent personal hygiene
- Ensuring nails are clean and short
- Re-reading this ERAS booklet
- Stocking up on paracetamol for your discharge home
- Watching our cardiac centre video
To do list
Below are some practical points to consider:
- I have informed relevant people of my admission to hospital
- I have all my medications to take with me
- I have all my belongings ready for my hospital stay (see list in information booklet)
- I have arranged my transport to and from hospital
- I have arranged someone to stay with me for a week following my discharge
- I have checked I have the correct support in place for my return home
- I know which medications I need to stop prior to my admission
- I have to shower using the body wash provided, on the day before admission. Please bring the bottle with you.
Patient diary
A patient diary is intended for your use while you are in hospital to give you the opportunity to take an active role in your care and assist you by enhancing your recovery. You will be able to record your thoughts and feelings throughout your hospital stay. It is also for recording your progress with the enhanced recovery goals of early nutrition and early mobilisation.
The diary is designed for you to complete but family, friends and members of the team looking after you can help you to fill it in if you need them to.
The diary sets out guidelines on what to expect on the days after your surgery. However, as everyone is an individual, you may vary slightly from the programme set out. This does not mean that you have failed, it is purely a variation to the programme.
We would like you to keep your diary when you go home, and complete the online evaluation of your stay (see last page).
Note: please refer to the PDF version of this booklet for the patient diary.
Hospital admission
Please bring your ERAS booklet and a pen.
If you are not Diabetic on the morning of your surgery, you will have a pre-operative carbohydrate drink. This is given 2 hours before your surgery.
To further aid your recovery whilst at home
- Continue to eat and drink well
- Shower every day and clean clothes every day. Use your own towel
- Pat, do not rub when drying wounds after showering
- Monitor wounds
- Take regular exercise as detailed in your patient information booklet
- Take part in your local Cardiac Rehabilitation
- Contact us if you have any worries/questions
It is common after heart surgery to retain excess fluid. Advice will be given on discharge regarding monitoring your weight if required.
If your weight goes up once at home, please seek the advice of your GP.
What to do if you have concerns after you have left hospital
Complications do not happen very often but it is important that you are aware of what to look out for.
In your patient information booklet you will find on page 26 – 28 advice regarding pain, infection control, wound care, irregular heart beat and other symptoms you may experience.
If you have any of the following symptoms:
- Your wound suddenly becomes red, swollen, painful or starts leaking discoloured fluid
- You notice you are coughing up more sputum or it is discoloured
- If your heart feels like it is racing or feels like it’s missing a beat (this is quite common following heart surgery) and you feel unwell when experiencing this or it is prolonged or happens frequently
Contacts
CICU
01273 696955
Ext. 64467
Cardiac Rehabilitation – Kay Hyde, Lead Specialist Nurse
01273 696955
Ext. 64157, 64009
This leaflet is intended for patients receiving care in Brighton & Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.