Download and print as a PDF (540kB pdf)
On this page
- What is this information about?
- Why have I been given this information?
- What and where is the prostate?
- What are Benign Prostatic Hyperplasia (BPH) and Bladder Outlet Obstruction (BOO)?
- How can HoLEP help me?
- What are the alternatives?
- What happens on the day of the procedure?
- What happens during the procedure?
- What happens after the procedure?
- When will I remove my urinary catheter?
- What will happen after my catheter removal?
- What should I expect when I get home?
- Can I do some exercises to improve my recovery after surgery?
- Do I need to make some lifestyle adjustments after surgery?
- What are the side-effects from this surgery?
- When will I be seen again?
- Where can I find further information or advice if I need it after I have read this information?
What is this information about?
This information provides a detailed overview of the prostate, conditions such as Benign Prostatic Hyperplasia (BPH) and Bladder Outlet Obstruction (BOO), and the HoLEP (Holmium Laser Enucleation of the Prostate) procedure.
It explains:
- the anatomy and function of the prostate
- the causes and symptoms of BPH and BOO
- the HoLEP procedure
- alternative treatments
- post-operative care
Why have I been given this information?
You have been given this information to:
- learn about prostate enlargement (BPH) and how it affects your urinary and overall health
- provide details about the HoLEP procedure, its benefits, risks, and alternatives, helping you decide if it’s the right treatment for you
- understand what to expect before, during, and after the procedure, including recovery and potential side effects
- explore alternative treatments and understand the potential outcomes of each
- provide contact details for your healthcare team and additional resources for ongoing support and information
What and where is the prostate?
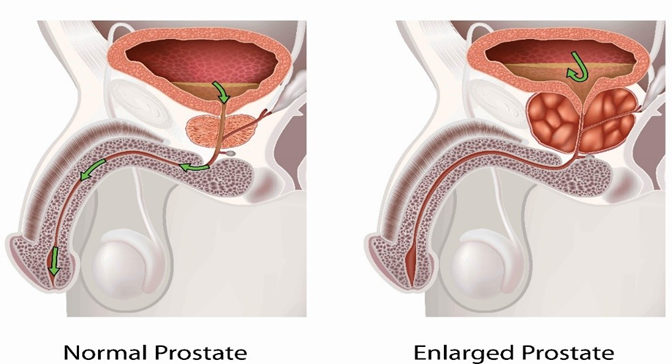
The prostate is a gland in the male reproductive system. Its main function is to produce fluid that protects and enriches sperm, which together with the sperm makes up semen.
The prostate is just below the bladder and above the muscles that help control urine flow.
Behind the prostate is the rectum, which allows doctors and nurses to check the prostate through an examination called a rectal exam. During this procedure, a doctor or nurse checks inside your bottom (anus and rectum) with their finger.
In young men, the prostate is about the size of a walnut and is shaped like a doughnut. It surrounds the urethra, the tube that carries urine out of the body.
The nerves that help with erections are also located around the prostate.
What are Benign Prostatic Hyperplasia (BPH) and Bladder Outlet Obstruction (BOO)?
Prostate enlargement (also known as hyperplasia) is when the prostate gland grows bigger but is not cancerous (benign). This is common as men age.
Benign Prostatic Hyperplasia (BPH) causes obstruction to the flow of urine from your bladder.
The prostate surrounds the bladder area and the urethra. As it becomes bigger, it squeezes and narrows the urethra, making it hard for urine to leave the bladder. This is called Bladder Outlet Obstruction (BOO).
This can cause a slow urine flow, a feeling of not fully emptying the bladder, and eventually, difficulty urinating, known as urinary retention.
How can HoLEP help me?
HoLEP (Holmium Laser Enucleation of the Prostate) is a procedure that uses a laser to remove enlarged prostate tissue.
Unlike the traditional method called Transurethral Resection of Prostate (TURP), which cuts away small pieces of the prostate, HoLEP allows the surgeon to peel the tissue (you can imagine this like an orange) off the prostatic body (that can be seen as the thick skin of the orange) in one large block. Please see image below.
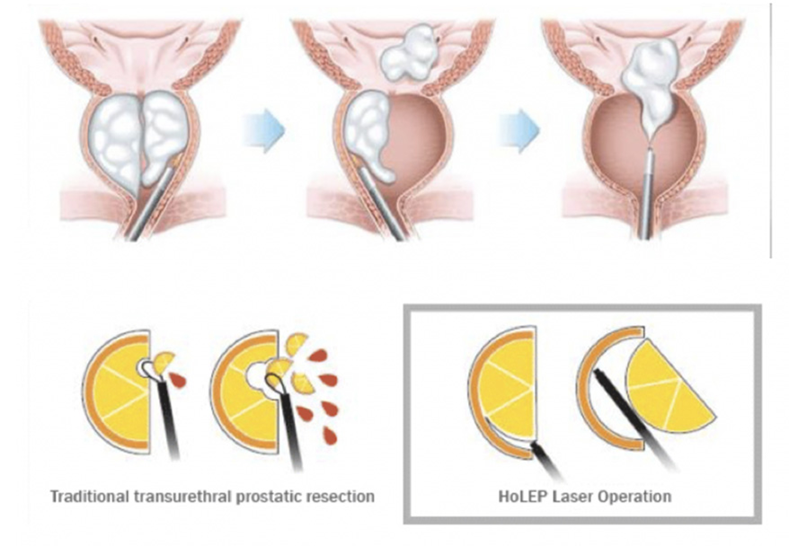
This piece is then broken up (morcellated) and removed from the bladder.
This creates a wider pathway for urine flow.
After the procedure, a catheter is inserted and usually removed either the same day or within 2–3 days.
What are the alternatives?
Here are some alternatives to consider:
- you can monitor your urine output, although this may require some lifestyle adjustments
- medications are available to improve urine flow, shrink the prostate, or both
- intermittent self-catheterization may be an option, or a long-term catheter can be inserted by your nurse
- surgical options are also available:
- minimally invasive procedures: Urolift (available locally), Rezum, iTind, and Aquablation (available with a referral)
- radiological option: Prostate artery embolization (PAE)
- open surgery.
Please ask the team for separate leaflets about these procedures if you would like more information.
What happens on the day of the procedure?
A urologist or a member of the urology team will see you before you go to theatre.
- they will briefly review your medical history and medications
- the details of the surgery will be explained again
- you will be asked to sign a consent form to confirm you understand the risks and are happy to proceed
You will also meet with an anaesthetist, who will:
- discuss the options of a general or spinal anaesthetic
- explain that a general anaesthetic is usually preferred for HoLEP, due to the length of the procedure and the need to remain still
- talk about pain relief after the surgery.
You will be asked to wear elasticated compression stockings to help reduce the risk of deep vein thrombosis (DVT), blood clots in the legs.
What happens during the procedure?
The operation is usually performed as a day case, provided there is a responsible adult at home to accompany you afterward (this is a requirement for same-day discharge).
In some cases, you may need to stay overnight, so please bring an overnight bag just in case. This will be discussed with your surgeon beforehand.
You will be given antibiotics before the surgery to reduce the risk of infection.
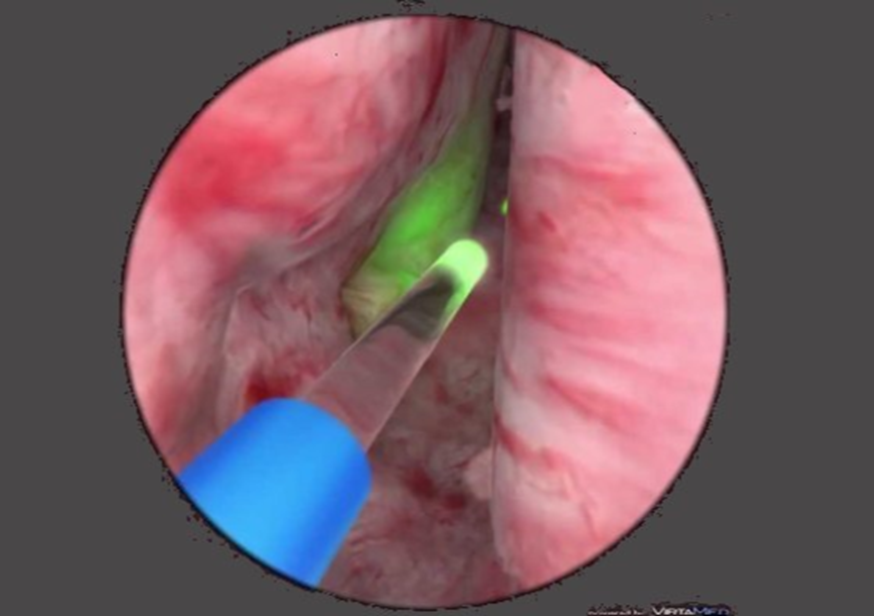
During the procedure, the surgeon will use a telescope (endoscope) to visualise the enlarged prostate.
The prostate tissue is then broken into small pieces (morcellated) and removed from the bladder.
The removed tissue will be sent to the laboratory for analysis to check for any signs of prostate cancer.
Results are typically available within 6 weeks.
A catheter will be placed in your bladder at the end of the procedure to allow bladder irrigation.
This involves flushing the bladder with salty water to wash out any clots or bleeding.
After surgery, you will be taken to the theatre recovery area, and once awake and stable, you’ll be transferred to the ward.
What happens after the procedure?
Once you’re on the ward, you will be able to eat and drink as normal.
Occasionally, you may receive intravenous fluids to keep you hydrated, but this will be stopped once you’re drinking well on your own.
As you drink more, the bladder irrigation will be gradually slowed down and eventually stopped.
If your urine is clear or light pink (“rose”), you’re drinking well, and there are no other concerns, you may be discharged the same day with the catheter still in place.
When will I remove my urinary catheter?
You will be invited back to the Urology Investigation and Treatment Centre (UITC) for catheter removal:
- This is typically on day 3 after surgery, based on the best chance of successful removal.
- In some cases, you may be asked to keep the catheter for up to 7 days.
- If you stay in hospital overnight, the catheter is usually removed the next morning.
What will happen after my catheter removal?
Your urine may be blood-stained, and it can be painful to pass urine initially.
You might feel the need to urinate frequently and urgently, but this usually improves over time.
Drinking plenty of fluids to keep your urine dilute and taking simple painkillers (e.g. paracetamol) can help relieve discomfort.
What should I expect when I get home?
It may take several weeks for you to fully recover from surgery.
Most patients feel tired for a week or two, and most men return to work 2 weeks after their operation. It is important to avoid heavy lifting and strenuous exercise and sport for the first 4 weeks.
A little bleeding can occur for at least 2 weeks, and some patients notice heavier bleeding around 2 and 4 weeks. This is due to small scabs separating from the cavity of the prostate as it heals (you may notice passing these when you pass urine).
Commonly, increasing your intake of fluids helps to control any minor bleeding, but if it persists beyond 24–48 hours, or if you experience severe bleeding, cannot pass urine, or feel unwell, then please contact your GP or go to A&E.
Improvements in bladder flow and emptying can be noticed quickly, but other symptoms might take more time to improve. For issues like waking up at night to use the bathroom, the surgery might not have much effect, as this problem can be caused by several factors.
Up to 1 in 10 men might experience temporary leakage after surgery and may need to use incontinence pads.
It is common to have some leaking when sneezing, coughing, or lifting things in the first 3 months after the surgery. This usually gets better over time as the pelvic floor muscles, which now handle bladder control, heal.
Can I do some exercises to improve my recovery after surgery?
Pelvic floor exercises are essential to strengthening those muscles and speeding up your continence recovery.
We recommend using the Squeezy app (or similar) to guide you through those and ensure you practise long and short squeezes, 8 repetitions, 3 times a day.
The risk of long-term leakage is around 1–2% (1 in 100 or 2 in 200) and goes up with certain risk factors (larger prostates, obesity, etc.).
Your surgeon will discuss this with you based on your personal situation.
Some men may have an overactive bladder after surgery, causing frequent, urgent trips to the bathroom or even accidents.
These symptoms usually get better within 6 months as your bladder adjusts. If these symptoms bother you a lot, let us or your GP know.
Do I need to make some lifestyle adjustments after surgery?
Yes, there are a few temporary changes you may need to make during your recovery:
- Medications and diet – Avoid caffeine and consider taking bladder-calming medications such as Solifenacin or Mirabegron for a few weeks, as advised by your doctor.
- Sexual activity – You can resume sexual activities once you feel comfortable, usually after 3–4 weeks. Don’t be alarmed if you notice blood-stained semen (red or pink); this can occur for several weeks post-operation.
- Driving – You may start driving again when you feel confident in your ability to make a safe emergency stop. This will vary from person to person.
- Alcohol – Avoid drinking alcohol until you are fully recovered, as it can irritate the bladder, slow healing, and interfere with medications.
What are the side-effects from this surgery?
These will be covered in detail during the multistage consent process between you and your surgeon (initially in clinic and again on the day of surgery); you should also have received plenty of relevant reading materials on the subject (further links included below).
Most men, however, mainly worry about the effect of surgery on their sexual function and continence:
Retrograde (dry) ejaculation
This occurs in nearly all men after HoLEP. Rather than sperm being ejaculated out through the penis during sexual climax, the sperm passes back into the bladder and is passed out in the urine. This will reduce the ability to have children but is not a means of contraception.
Erectile dysfunction (ED) (also known as impotence)
The risk of ED is classically quoted at ~1% (1 in 100) as the laser penetration is shallow and the risk of injury to the nerves responsible for erections (that run on the outside of the prostate) is low.
If you do not already have ED, you are unlikely to develop it after prostate surgery. However, if you already have ED, the surgery will not improve it.
If this becomes a problem, treatments will be available through your GP (Viagra, Cialis, or Tadalafil), creams, pellets, or vacuum devices.
Incontinence
Temporary loss of urinary control is common after the procedure. This can include stress incontinence and overactive bladder symptoms. To recover quickly, do pelvic floor exercises regularly, drink enough water, and limit caffeine.
When will I be seen again?
You will have a follow-up appointment at the outpatient clinic approximately 3 months after your surgery to assess the effects. This allows time for your symptoms to stabilise.
The results of any removed tissue will be ready within 6 weeks. If there are any unexpected findings, we will schedule an earlier appointment to discuss them with you in person.
Where can I find further information or advice if I need it after I have read this information?
Useful further reading
Useful telephone numbers
The Princess Royal Hospital
The Urology Nursing Team
01444 441881
Ext. 65457
Urology Consultants
Ms Blach’s secretary
01444 441881
Ext. 67810
Mr Coker’s secretary
01444 441881
Ext. 68043
Mr Crawford’s secretary
01444 441881
Ext. 67808
Mr Symes’ secretary
01444 441881
Ext. 67809
Mr Larner’s secretary
01444 441881
Ext. 67808
Mr Alanbuki’s secretary
01444 441881
Ext. 67810
Mr Zakikhani’s secretary
01444 441881
Ext. 67809
Mr Good’s secretary
01444 441881
Ext. 67808
This leaflet is intended for patients receiving care in Brighton and Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.
Today’s research is tomorrow’s treatments. That’s why UHSx is proud to be a research-active Trust. Find out how you can get involved.
Visit our website www.uhsussex.nhs.uk/research-and-innovation/information-for-patients-and