Download and print as a PDF (343kB pdf)
On this page
- What is the Ductus Arteriosus?
- What is Patent Ductus Arteriosus?
- What are the signs and symptoms?
- How is a PDA diagnosed?
- How is a PDA initially managed?
- What treatment is available?
- What alternative treatment is available or may be needed?
- What happens after treatment?
- What about follow up?
- Where can I get additional support?
- Who should I ask if I have further questions?
What is the Ductus Arteriosus?
The Ductus Arteriosus is a small muscular blood vessel that joins the pulmonary artery (main artery to the lungs) to the aorta (main artery to the body). This naturally occurring connection allows blood to be diverted away from the lungs whilst the baby develops in the womb, as the lungs are not needed before birth. The lungs are only used to breathe once the baby has been born. After birth the duct begins to close and is usually completely closed within a couple of days in full term babies. The duct may remain open in premature babies and this is called a Patent Ductus Arteriosus (PDA).
The heart has four chambers. Two ‘receiving’ chambers: these are called the right and left atriums. Two ‘pumping’ chambers: these are called the right and left ventricles. The pulmonary artery and aorta come from the ventricles.
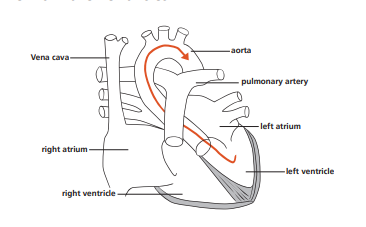
This is a diagram of the normal heart. Oxygen rich blood flows from the left ventricle, into the aorta, and then out to the rest of the body. Oxygen-poor blood flows from the body into the right atrium then the right ventricle and into the pulmonary artery to the lungs to collect fresh oxygen (oxygenation).
After oxygenation, oxygen rich blood comes back to the left atrium and into the left ventricle. Blood is then pumped into the aorta to supply the rest of the body. If the duct closes normally there is no connection between the aorta and pulmonary artery.
What is Patent Ductus Arteriosus?
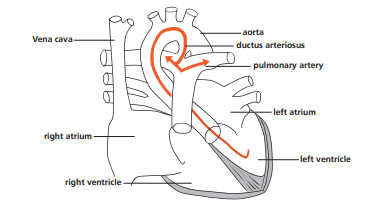
This is a diagram of a heart with a PDA (Patent Ductus Arteriosus). The duct between the aorta and pulmonary artery is still open and let’s blood flow from the left ventricle, into the aorta, and then back into the pulmonary artery. This increases the blood flow to the lungs.
What are the signs and symptoms?
The effects of a PDA on the baby may be:
Increased work of breathing: faster breathing rate, needing more oxygen to keep oxygen levels in the blood stable, desaturations: drop in the measured oxygen content in the blood, apnoea: not breathing for approximately more than 10 to 20 seconds.
Fluid in the lungs: extra blood is flowing to the lungs instead of around the body.
Increased work for the heart to do: murmur, faster heart rate.
This is because a lot of blood flows back into the lungs and then back to the heart without supplying the rest of the body. This means the heart has to work harder.
You may find the nurses describe your baby in some of these ways:
• The doctor has heard a murmur.
• Your baby is quieter than usual.
• Your baby doesn’t like being handled as usual.
• Your baby has needed a bit more oxygen because the oxygen level has dropped in the blood supply.
• Your baby is working harder to breathe.
• Your baby hasn’t gained weight.
How is a PDA diagnosed?
The doctor will examine your baby by listening to the heart, talking to the nurses, reviewing the observations (heart rate, breathing rate and blood pressure), checking blood results and taking a chest x-ray of your baby.
If a PDA is suspected it may be confirmed with an ultrasound examination called an echocardiogram (or simply called ‘echo’). This examination is similar to the ultrasound you had when you were pregnant. It is able to show how the blood is flowing through your baby’s heart.
How is a PDA initially managed?
We may feed your baby smaller amounts. This will help to reduce the excess fluid in the lungs.
Your baby may need to have some help with their breathing.
They may have:
• Oxygen via small prongs inserted in the nose.
• Via a CPAP machine: small prongs deliver oxygen under controlled pressure through the nose.
• Via Optiflow: small prongs deliver oxygen via low flow through the nose.
Your baby may need some medication to help lose some of the extra fluid. Diuretics help the body to remove extra fluid by producing more urine.
What treatment is available?
The PDA can often be closed using medicines called Indomethacin, Ibuprofen or Paracetamol. Indomethacin is given through a vein as an infusion over 36 hours while Ibuprofen and Paracetamol are given as a short course over 3 days. The doctors will do further echo’s to see how the duct is responding to the medication. Ibuprofen is known to have some side effects such as reduction of blood flow to kidneys and bowel as well as reducing platelet function, which may reduce the ability to stop bleeding. Your baby will be closely monitored for any side effects which are usually reversible.
Doctors and nurses will check your baby’s kidney function and platelet count with regular blood tests. They will weigh your baby and measure urine output daily to check their kidney function. To check the gut is also functioning well, nurses will check that feeds are being absorbed by looking at the amount of feed left in the stomach before a next feed. The doctors would be happy to discuss this with you.
What alternative treatment is available or may be needed?
If the PDA does not respond to medication the doctors will discuss further treatment with you. Your baby may need to have surgery to correct the PDA. This operation closes the duct with a metal clip. The operation is carried out through a cut in the left side of the chest and the clip is then put around the duct to close it.
Surgery is carried out either at Evelina Children’s hospital, St Thomas’s in London or at Southampton Hospital. Your baby will be taken to this hospital by the Neonatal Transport Service who will collect them again afterwards.
The surgery is usually carried out on one day and then your baby returns to Brighton as soon as they are stable. You will need to travel up to St Thomas’s or Southampton to see the surgeons and sign the consent form. A parent may travel in the ambulance with their baby.
The Cardiac surgeons will explain what will happen to your baby there and then the doctors here in Brighton will continue your baby’s care when they return.
What happens after treatment?
You may find it takes a while for your baby to show complete improvement following surgery because they need to adjust to the new way their body works now the duct has been closed.
They have just had an operation and they have just had two long journeys in an ambulance. Their condition will continue to be checked regularly by the nurses and doctors on the unit. Most babies do well following the operation.
What about follow up?
Your baby will be followed up in the outpatients department to monitor their growth and development. There is no need for any cardiac follow up appointments.
Where can I get additional support?
You can talk to your baby’s doctors and nurses for additional information. If you need an interpreter the nurses can arrange for one to be present. Interpreters for the deaf or hard of hearing are also available on request. If you would like to seek support from the counsellor attached to the unit do let the staff know.
The British Heart Foundation is a useful source of support.
British Heart Foundation
02079 350185
Who should I ask if I have further questions?
The nurse and neonatal team looking after your baby will be happy to answer any further questions you may have.
References
Heart line Association. 1989. Heart Children, A practical handbook for
parents. Heart Line Association.
Trevor Mann Baby Unit, The Royal Sussex County Hospital, Eastern Road, Brighton BN2 5BE
01273 696955
Ext. 64377
This leaflet is intended for patients receiving care in Brighton and Hove or Haywards Heath.
The information in this leaflet is for guidance purposes only and is in no way intended to replace professional clinical advice by a qualified practitioner.