On this page
- What is a tracheostomy?
- What does a tracheostomy do?
- What are the alternatives to a tracheostomy?
- What are the benefits of having a tracheostomy instead of an endotracheal tube?
- How is a tracheostomy performed?
- What happens after the tracheostomy is removed?
- What are the risks of having a tracheostomy?
- Common risks
- Uncommon risks
- Further sources of information and advice
What is a tracheostomy?
A tracheostomy is a hole made in the front of the windpipe below the larynx.
A plastic tube is inserted through this hole and may be connected to a ventilator.
What does a tracheostomy do?
A tracheostomy allows the person to breathe when they are unable to breathe normally for themselves. This may be because:
- they have an injury
- their muscles are too weak
- their airway is blocked by something such as swelling or a tumour.
What are the alternatives to a tracheostomy?
A breathing tube through the mouth (called an endotracheal tube) is a good option for patients who need ventilation for a short period of time.
However, it can cause damage to the mouth, throat, and larynx and make it difficult to keep the mouth and teeth clean. It normally also requires the patient to be sedated.
If patients need the support of a ventilator for a longer period, a tracheostomy is often recommended.
What are the benefits of having a tracheostomy instead of an endotracheal tube?
- A tracheostomy is generally much more comfortable for patients. This means that sedatives can be reduced or stopped, which allows patients to be more awake.
- Some patients can have a valve fitted into their tracheostomy to allow them to speak.
- A tracheostomy is placed below the vocal cords, so the vocal cords will not get damaged (this can happen with an endotracheal tube).
- A tracheostomy speeds up rehabilitation (getting stronger and more independent). Patients can slowly get used to coming off the ventilator, take in more nutrition, and get stronger once a tracheostomy is placed.
All these things can improve patients’ strength and speed up their recovery.
How is a tracheostomy performed?
There are two ways to do a tracheostomy. One is through the skin (also called percutaneously) and the other is surgically.
A percutaneous tracheostomy is performed in the intensive care unit. A needle is inserted into the front of the neck, a guide wire is passed through it and into the windpipe. The hole is then stretched so that a plastic breathing tube can fit into the windpipe and then be connected to the ventilator.
The surgical method is performed in an operating theatre. It involves a larger cut in the front of the neck and direct access to the windpipe.
Both methods are safe. They are done under general anaesthetic. The medical team will decide which method is best for each patient.
Once a tracheostomy has been inserted there will be a sign above the patient’s bed which will remain there for as long as the tracheostomy is in place. This sign provides key information about the type of tracheostomy that is in place and is an important safety feature.
What happens after the tracheostomy is removed?
Once the tracheostomy is no longer needed it will be removed and a dressing placed over the hole.
The hole can be stitched if needed and will eventually heal over.
The tracheostomy can sometimes cause scarring inside the windpipe which can make the windpipe narrower. This is known as tracheal stenosis.
Tracheal stenosis can occasionally cause breathing difficulties. Stenosis is quite common, but only three to 12 percent of patients with stenosis need an intervention to help with this. If this happens, surgery to widen the windpipe may be needed.
What are the risks of having a tracheostomy?
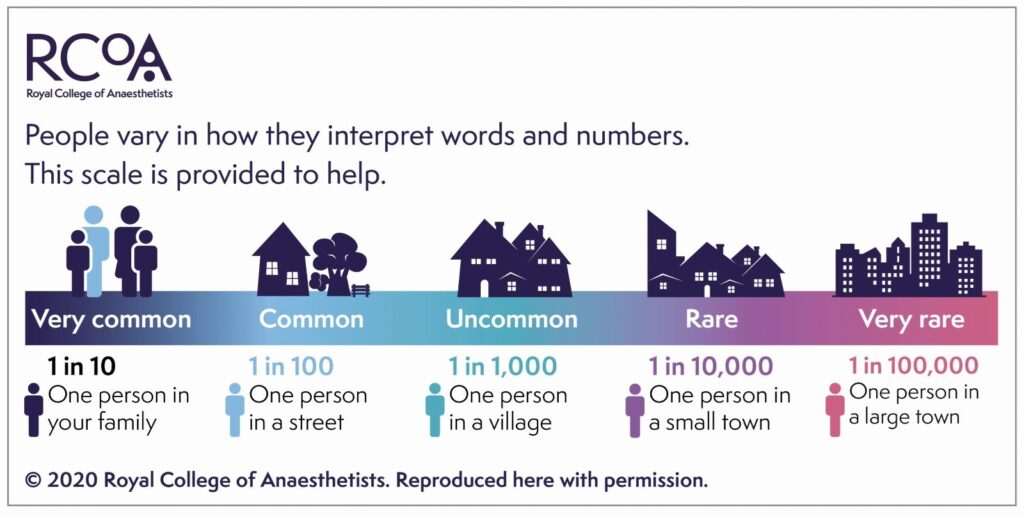
Common risks
- Scarring: once a tracheostomy has been removed, there will be a small scar.
- Bleeding: there are blood vessels near the windpipe around where a tracheostomy is inserted. Bleeding is common but usually minor. Very rarely it may require a blood transfusion or a further procedure to stop it.
- Infection: the tracheostomy is inserted in a sterile way but as with any procedure there is a risk of infection. Serious infections are rare.
- Blockage: the inner tube of a tracheostomy can become blocked and cause difficulties in breathing. The tube can be suctioned or replaced to clear the airway.
- Dislodgement (accidentally taken out): the tracheostomy tube can sometimes become accidentally removed during transport, if the patient is turned or moved in bed, or if they have another procedure. It can also become dislodged if the patient coughs a lot or takes it out themselves.
If this happens within 10 days of first being put in, patients may need to be intubated again with a tube in their mouth because the tracheostomy tract has not fully formed. If it is after 10 days, the tracheostomy tube can usually be replaced easily without further complication.
Uncommon risks
- Accidental Injury: There is a risk of damage to nerves that run near the windpipe as well as to the oesophagus which can affect speech and swallowing.
- Pneumothorax: This is where the lung collapses because air has leaked from the airways into the space surrounding the lung. This can occur, though rarely, during tracheostomy insertion. It may require another tube to be placed into the chest to drain the air and reinflate the lung.
- Tracheoarterial fistula: Rarely, a connection can form over time between the tracheostomy and a blood vessel. This does not happen frequently but is a serious complication and can lead to severe bleeding.
- Death: If some of the risks listed above cannot be resolved or are particularly severe there is the possibility of death occurring directly related to a tracheostomy. This occurs rarely at a rate of approximately 1 in 600 tracheostomies.
Further sources of information and advice
If you have any questions about anything contained in this leaflet or about tracheostomies in general, please ask your medical team. You can call 01273 696955, extension 63095.
This information is intended for patients receiving care Brighton or Haywards Heath.