Download and print as a PDF (659kB pdf)
On this page
- Why have I been given this information?
- What is this information about?
- Why is it important that I read this information and follow the advice?
- My Surgery Timeline
- What can I do to plan and prepare for my bariatric surgery?
- Liver reduction diet (LRD)
- What, and when, should I eat after surgery?
- How should I eat and drink after my operation?
- What other changes or side effects might I experience because I have had bariatric surgery?
- Why is it important for me to exercise after my bariatric surgery?
- Frequently asked questions
- Useful resources
Why have I been given this information?
You have been given this information because you have chosen to have your bariatric surgery at St. Richard’s Hospital.
What is this information about?
This information will help you prepare for your surgery and tells you about the long-term lifestyle changes that you will need to make after surgery.
Why is it important that I read this information and follow the advice?
Being prepared helps you to adapt to life after surgery and gives you the best possible chance of long-term success. Please take time to read this booklet carefully.
More information can be found on our website, including patient videos.
My Surgery Timeline
Who will I see:
| Six weeks after the operation? | Appointment with nurse |
| Three months after the operation? | Appointment with dietitian |
| Six months after the operation? | Appointment with dietitian |
| One year after the operation year? | Appointment with dietitian and you will have a blood test |
| 18 months after the operation? | Appointment with dietitian |
| Two years after the operation? | Appointment with dietitian and you will have a blood test |
What can I do to plan and prepare for my bariatric surgery?
There are things that you can start to do now which will help you adapt and stay on track after your surgery:
- Stop smoking. Ask your local smoking cessation team for support.
- Start exercising. Try and build this into your weekly routine. Find something that is manageable for you.
- Eat regularly. Aim for three meals per day. You may need to plan ahead to achieve this.
- Practice mindful eating. Concentrate on your meal, chew thoroughly and avoid distractions when you are eating
- Build a support network. For example:
- friends
- family
- work colleagues
- online forums
- a local support group
- Take the recommended vitamin and mineral supplements. This is usually one multivitamin and mineral tablet and one Vitamin D tablet per day before surgery.
- Think about how you will cope with eating food when outside the home, including social events.
How can I make healthy lifestyle changes?
It is difficult to break old habits and make healthy lifestyle changes.
- Focus on one thing at a time. It can be overwhelming trying to change too much at once.
- Set yourself small goals. Writing these down and keeping track of your progress can help.
- Do not just set yourself weight loss goals. Focus on the habits that you would like to change.
How much weight might I lose?
Weight loss after surgery is different for everyone. Weight loss will be affected by:
- diet
- activity levels
- age
- habits
Do not expect that your Body Mass Index (BMI) will fall into the healthy range (18.5 to 25) after surgery. This is not something you should aim for.
You will lose weight very quickly in the first three months after surgery. It is then normal for weight loss to slow. You will also have some weeks where you will not lose any weight and your weight loss will stall. Most people will find that they stop losing weight around one year after surgery. It is unusual to continue to lose weight after this.
Putting on a small amount of weight is normal. Around one in five people will put on a significant amount of weight following their surgery. The reason people regain lots of weight is complicated. All you can do, and all that we expect, is to try your best. This means following the advice from your bariatric surgery team. It is essential that you stick to lifelong healthy eating and activity habits to maintain weight loss. Your total weight loss might not match with your hopes and wishes which can be hard to accept. Speak to your team about a realistic weight loss target.
Weight loss is affected by age, activity level, dietary discipline, and basal metabolic rate. Some people lose more weight than expected, some lose less. It is difficult to predict.
Liver reduction diet (LRD)
What is an LRD diet?
An LRD is a diet low in calories and carbohydrates. It is also known as a milk diet.
Be aware
You must only drink milk for two weeks and not eat any food. This gives you enough nutrition to keep you well. It is likely you will lose weight, but it is not a diet for weight loss.
Why do I need to follow this diet?
This diet shrinks the size of your liver as you are eating less calories and carbohydrates. This is important because it means that it is easier for the surgeon to reach your stomach and do your operation safely with less chance of damage to your liver.
How long do I need to follow the diet for?
You will need to follow this diet for two weeks before your surgery. Some people will need to follow this diet for up to three weeks, but we will tell you if you need to do this.
What is the risk of not following the diet?
Your surgery will be stopped if your liver is too large, and it is not safe to continue with the operation.
What can I have late in the night before my surgery and on the day of my operation?
- From midnight on the night before your surgery you can drink clear fluids. For example, water, black tea, black coffee, no added sugar squash
- On the day of your operation from either 6.30am or 11.30am (this depends on the time of your operation) you will not be able to eat or drink anything (nil by mouth).
What happens if I am on the LRD and I have diabetes?
You will only be taking 120g of carbohydrate a day while you are on the milk diet. This means some of your diabetes medication may need to change. The nurse will advise you of any changes to your diabetes medications and adjustments to your dose of insulin. If you take insulin or oral medications that can cause low blood sugar (hypoglycaemia), you need to check your blood sugar levels at least four times a day.
What side effects might I have because I am on the LRD?
- Diarrhoea (runny poo)
If you have diarrhoea, swap to lactose free milk (semi skimmed). If this does not improve your symptoms, you could take loperamide (Imodium) medication which you can get from a pharmacy. If you need to you can contact the bariatric team for advice.
- Constipation (difficulty pooing or very hard poos)
This is the most common side effect of the milk diet. We recommend you take milk of magnesia, laxido, senna, or Movicol to relieve these symptoms.
Do not arrive for surgery constipated.
Is there an alternative to this diet to reduce the size of my liver?
Research tells us that the milk diet gives the best results. If the milk diet is not suitable, you should speak to your bariatric surgery team for advice.
What am I allowed when I am on the LRD?
You cannot have any food.
Every day you can have the following:
- 4 pints (2 litres) of either semi-skimmed cow’s milk, lactose free milk or soya original. Be aware that alternative milks such as oat, almond or rice milk are not suitable.
- 2 pints (1 litre) of calorie free fluid. This includes water, tea, coffee and no added-sugar squash
- 1 salty drink. For example, Marmite, Bovril, stock cube or 1tsp salt in squash
- 1 multivitamin and mineral tablet. For example, Sanatogen A-Z or a supermarket A-Z
What else am I allowed when I am on the LRD?
Drinks:
- water
- tea, coffee or herbal tea (no added sugar)
- no added sugar squash
Extras:
- no added sugar Crusha or Skinny Syrups can be added to milk
- one sachet (1 pint) or 5 x 115g pots of ready to eat sugar free jelly a day
- chewing gum (maximum 3 pieces per day)
What tips can help me when I am on the LRD?
- Keep your milk separate from anyone else’s at home and work.
- Use sweeteners instead of sugar in tea and coffee.
- Plan your routine for fitting in all of your fluids.
- Consider how the milk diet may affect your family and what support you will need. For example, who will do the cooking.
- Think about how you might cope with following the milk diet at work or special occasions.
- Remove tempting foods from the house as much as possible.
Be aware, the LRD:
- is preparation for surgery, not for weight loss
- should only be used under supervision from your dietitian
Please contact the dietitian if you suffer any side effects from this diet.
What, and when, should I eat after surgery?
Textured foods need to be introduced gradually to allow for healing and for your new stomach to adapt.
Stage 1: pureed consistency (weeks 0 to 4)
No lumps. Smooth like the consistency of a yoghurt.
- Do not eat and drink more than 4tbsp or 100 to 200ml at a time.
- You will need a blender or liquidiser and a sieve to prepare your food.
- Add a liquid to help make your food a smooth consistency. For example, tomato puree, gravy, stock, or milk.
- Puree and serve the protein part of your meal separately from the vegetable or potato to give you different flavours on your plate.
- You may not feel up to cooking after your operation. Be prepared by cooking, blending and freezing food before your surgery.
- Freeze pureed food in ice cube trays. This helps you get familiar with portion sizes without causing waste.
Meal ideas
The following meal ideas can all be pureed to achieve a smooth consistency:
Breakfast:
- Ready brek; Weetabix (with milk)
- plain or Greek yoghurt with pureed fruit
- pureed poached egg
Lunch:
- soup with no lumps. Include a protein source. For example, chicken, beef, lentil, beans
- pureed cottage cheese; tinned fish; silken tofu; low sugar baked beans or poached egg with pureed steamed vegetables and mashed potato
Dinner (all to be pureed):
- shepherd’s pie
- fish pie
- casserole, mild chilli, stew or, Bolognese sauce
- cauliflower cheese
- dahl
Snacks:
- cheese triangle
- smooth peanut butter
- natural or Greek yoghurt or Skyr
- Hummus
- low sugar custard
- meat or fish pate
- milky drink
Stage 2: mashed/crunchy consistency (5 to 8 weeks)
This is the bridge between pureed foods and normal textures.
- Practice eating in a way that will result in a good long-term weight loss.
- If you experience discomfort, try to work out why. For example, did you eat too much or eat too fast? Did you chew your food enough?
- At first, you will be able to tolerate foods better if they are soft and wet. Adding gravy or sauces can help.
- The “fork test” can be used to check the texture. If your fork passes easily through the food, it is the right texture for stage 2. If you have to force a fork through your food, it is best avoided at this stage.
Meal ideas
Breakfast:
- porridge
- low-sugar cereal such as Weetabix or Cornflakes
- Melba toast with peanut butter, cream cheese or hummus
- scrambled egg with avocado
Lunch:
- crackers or Ryvita with cottage cheese, cheese triangle, scrambled egg, or pate
- jacket potato (no skin) with tinned fish, baked beans or chilli
- couscous with cooked vegetables and lentils
- omelette
Dinner:
These no longer need to be pureed; shepherd’s pie, fish pie, casserole, mild chilli, stew, Bolognese sauce, cauliflower cheese, dahl, curry.
Snacks:
- wholegrain crackers or rice cakes with peanut butter, pate or cream cheese
- soft fruit
- yoghurt
Stage 3: normal consistency (9 to 12 weeks)
Do start trying to eat different textured foods as it is now safe to do so.
- There will still be some foods that you cannot tolerate. Bread, pasta, rice and dry meats are the foods which are usually most difficult to tolerate. Take things slowly. Add one new food at a time.
- From about 10 to 12 weeks you can try salads.
- Try to avoid soft or sloppy food as it is easy to eat too much of these.
- Please experiment carefully to see what you can tolerate. This varies from person to person. Foods that you could not manage at the beginning will be tolerated at a later date. Try again 1 to 2 weeks later.
Meal ideas
Breakfast:
- breakfast cereal. For example, Weetabix, Shredded Wheat, porridge, overnight oats
- toast with peanut butter
- omelette
Lunch:
- toasted pitta, sandwich thin or wrap with protein source such as meat, fish, hummus or cheese and salad
- beanburger with couscous
- jacket potato with tuna or low sugar baked beans
- fishcakes with steamed broccoli
- frittata
- lentil and feta salad
Dinner
- stir fry with chicken, tofu, cashews, prawns or Quorn and vegetables
- pitta with falafel, hummus and salad
- bean or meat tagine
- fillet of fish with steamed vegetables and new potatoes
- roast meat with roast vegetables
- chickpea curry
Snacks:
- wholegrain crackers
- apple slices with peanut butter
- small portion of fruit
- yoghurt
- 30g of plain nuts
- slice of cold meat
- 20g cheese
- vegetable sticks with hummus
How should I eat and drink after my operation?
Be aware
How you eat and drink is just as important as what you eat and drink.
Speed
A main meal should last 20 to 30 minutes. If it takes less time than this, you are eating too quickly. This can lead to pain, discomfort and bringing your food back up (regurgitation). Putting your fork down between each mouthful can help you eat slowly.
If your meal is taking longer than 30 minutes, you may be trying to eat too much food. You should not continue to pick at your meal after 30 minutes.
Chewing
Before your operation, your stomach would churn your food to break it down for digestion. Now your chewing must do that job. Each mouthful should be about the size of a 20p piece. Chew every mouthful 20 times, until food is smooth with no lumps, before swallowing.
Calm atmosphere
Set aside times for your meals and snacks. Create a calm environment with no distractions. Take your time to eat so you can enjoy your food and feel satisfied. This will also help you to eat correctly.
Amount of food and meal patterns
The amount (volume) of food and fluid your stomach can tolerate will be much smaller after surgery. At first, you will only manage 2 to 4 tbsp, or 100 to 200mls at a time. You must eat six times a day for at least the first eight weeks after surgery. Ensure a regular eating pattern and avoid long periods of fasting.
As the months go by, you will be able to eat more at each meal. It is important to stop eating when you are full. Over-eating can cause you to be sick or to feel uncomfortable. This behaviour may result in poor long term weight loss.
Your portion size should not be more than a tea plate (15cm). It is important that you do not have larger portions than this. Long term, a typical meal pattern should be three main meals and two to three small snacks a day.
Eating well takes careful planning. Be aware of inappropriate snacks creeping in.
Eat protein foods first
Rapid weight loss can cause loss of muscle mass, weakness and reduced immune function. Protein is one of the building blocks for every cell in your body and needs to be the main component of your diet, especially in the early stages.
Make sure you eat your protein food first. Good protein sources include fish, chicken, beef, lamb, pork, eggs, pulses (peas, beans, lentils), nuts, seitan, cheese, milk, yoghurt, fromage frais, soya alternatives, tofu, and Quorn.
Fluids
Not drinking enough can make you dehydrated. This can cause low energy levels, headaches, and dizziness. Aim for a minimum of 2 litres (8 cups) of fluid a day. You must sip slowly throughout the day. You will not be able to gulp drinks when thirsty or in a hurry as this will cause pain.
Avoid drinking and eating at the same time. Do not drink for 30 minutes before or after food.
Be aware
Alcohol is not recommended during the first year after surgery because of its high calorie content and because there is a risk of developing alcohol dependency after surgery.
If you do try alcohol, you should be aware that you are likely to feel the effects quickly. Drinking alcohol regularly may stop you achieving your goals.
What other changes or side effects might I experience because I have had bariatric surgery?
Dumping syndrome
Dumping syndrome is caused by food moving quickly through the gut. If you eat foods which are high in sugar, the sugar is taken into your blood very quickly and this can cause you to have high blood sugar (hyperglycaemia).
Symptoms of dumping syndrome include:
- feeling sick or being sick
- sweating
- dizziness
- diarrhoea
To avoid dumping syndrome, try not to have high sugar foods such as chocolates, sweets, cakes, desserts, biscuits, and fruit juices. There are hidden sugars in lots of foods, so it is sensible to check food labels. As a guide, aim to avoid foods with more than 5g sugar per 100g in the food or drink.
If you have any of the symptoms of dumping syndrome, first have a rest. Then try to work out what caused them and whether it could be because you’ve eaten foods which are high in sugar. This can help prevent you from getting the symptoms again.
Fertility and pregnancy
Being overweight can prevent ovulation and make it less likely that you will get pregnant. This can change with weight loss. For this reason, you should consider which type of contraception you wish to use after your surgery. Contraceptive pills are less likely to stop you from getting pregnant after gastric bypass surgery. We recommend you use a different contraceptive such as a depo injection, barrier method (cap or condom) or a coil. Ask your GP to advise you about this.
Avoid getting pregnant for the first year after your bariatric surgery.
A man’s fertility will also increase following weight loss.
Hair loss
Rapid weight loss after surgery can result in hair loss. This usually happens three to six months after surgery. It typically lasts for around three months, but it can take some time for your hair to recover. Your dietitian will monitor your food intake and advise accordingly. Taking your recommended vitamins is essential, but there is no need to buy any specific supplements for hair re-growth.
Bowels
Your bowel habits can change after surgery.
You may have diarrhoea as you are not taking in nutrients as well, and the flow of food through your gut is much quicker.
You may have constipation if:
- you are not getting enough liquid from what you are eating and drinking (your fluid intake is low)
- your fibre intake is low
- your body is used to needing laxatives
- you are inactive
- you are taking painkillers.
If you have any concerns, please discuss this with the team.
Weight regain
Some patients do not lose a lot of weight or will regain weight. Conditions like diabetes, sleep apnoea and high blood pressure that might have gone away or got better (been in remission) can become a problem again.
To give yourself the best opportunity to achieve your goals:
- be well prepared before surgery
- attend all your appointments
- follow the advice of your bariatric team
Be aware
This surgery does not “cure” weight issues. Your weight will always need monitoring and it will take effort and discipline from you to keep your weight lower than it was before your surgery.
Depression and eating disorders
Surgery is challenging. You may suffer psychologically after the surgery, particularly in dealing with your new body image and your emotional relationship with food. People with underlying eating disorders may develop new eating disorders.
Do please discuss these challenges with your team who can direct you to the best support.
Why is it important for me to exercise after my bariatric surgery?
Exercise will help keep muscle tone, support weight loss, and improve mental health.
Try to start with a small goal, for example a walking plan. Walking is good as it is a weight bearing exercise and can help protect your bones from becoming weak (osteoporosis).
Over time, you will be able to build up your stamina and move on to other forms of activity. If you suffer with joint pain, exercises that you do in the water, such as swimming or aqua aerobics are more suitable. These put less pressure on your joints.
Frequently asked questions
I have a problem being sick after eating. What do I do?
It might take time for you to get used to the new ways of eating and follow the eating advice. If you produce white froth from your mouth or regurgitate food after eating, consider the following:
- did I eat too quickly?
- did I chew it well enough?
- was it too soon after surgery to have the food I was eating?
- did I eat too much?
If you are being sick often over two to three days contact your bariatric team for advice.
What can I do if I get constipated?
If you get constipated, first check that you are drinking enough fluids and eating enough fibre.
You can take a laxative if constipation is a problem. For example, milk of magnesia, lactulose, laxido, senna, or Movicol.
It is also important to be as active as possible.
What can I do if I get runny poos (diarrhoea)?
Do think about what might have given you diarrhoea.
You may get diarrhoea if you have:
- a tummy bug
- recently taken medicines to treat an infection (antibiotics)
- dumping syndrome caused by eating food high in sugar
If you have diarrhoea often for more than a week, contact your bariatric team for advice.
Do I have to follow the puree diet for four weeks?
Yes. Your gut is healing from the surgery during this stage. It is important to be confident with each stage before you progress onto the next.
Can I eat baby food on the puree stage?
No. Baby food does not provide enough nutrition for adults.
Should I take protein shakes?
No. You can get enough protein by planning what you eat and following the advice in this guidance.
Why haven’t I lost any weight?
Do not weigh yourself every day. Our advice is to wait for the nurse to weigh you at the appointment you will have six weeks after your operation. In the weeks following your surgery your body is recovering. You might not lose weight every week. Make sure you are eating six times a day and drinking enough fluid.
How much can I eat?
Your portion sizes increase gradually from 2 tablespoons per meal to a side plate over the first six months. It can be difficult not to finish everything on your plate, but you should stop eating when your tummy feels full. Do remember to serve small portions to avoid wasting food.
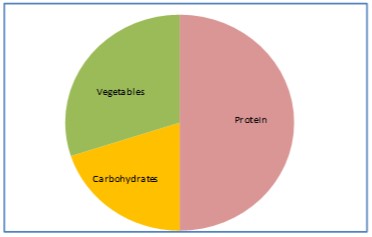
Main meals should be about the size of a side plate (this is about the size of your hand span) and include protein, vegetables and starchy carbohydrates in the proportions shown below.
Vitamin and mineral tablets
After surgery you will be unable to meet your vitamin and mineral needs from your diet alone. This is because you will only be able to eat small amounts of food. You will need to take vitamin and mineral tablets for life. You will need to buy them yourself as your GP will not prescribe these for you.
You need:
- multivitamin & mineral
- calcium
- vitamin D3
- iron
- vitamin B12 (one injection every three months, provided by your GP)
Please read the leaflet ‘Vitamin & minerals for life after bariatric surgery’ for detailed vitamin and mineral recommendations.
Blood tests
You should have a blood test at least once a year. While you are under the care of the bariatric team at St. Richard’s Hospital, you will have your yearly blood test at your appointment with the dietitian. Once you are discharged from St. Richard’s (usually two years after surgery) you will need to arrange for your GP to give you a blood test every year.
Useful resources
Books
Please see the PDF version of this leaflet to see the book titles and front covers.
Apps
- Baribuddy
- NHS food scanner
- NHS active 10
Websites
Bariatric Surgery Service
Bariatric Surgery Service, St Richard’s Hospital, Spitalfield Lane, Chichester, West Sussex, PO19 6SE.
Phone
01243 831655
We are committed to making our publications as accessible as possible. If you need this document in an alternative format, for example, large print, Braille or a language other than English, please contact the Communications Office by emailing [email protected] or speak to a Bariatric Dietitian.